A 200-Year Journey of America’s First Specialty Hospital
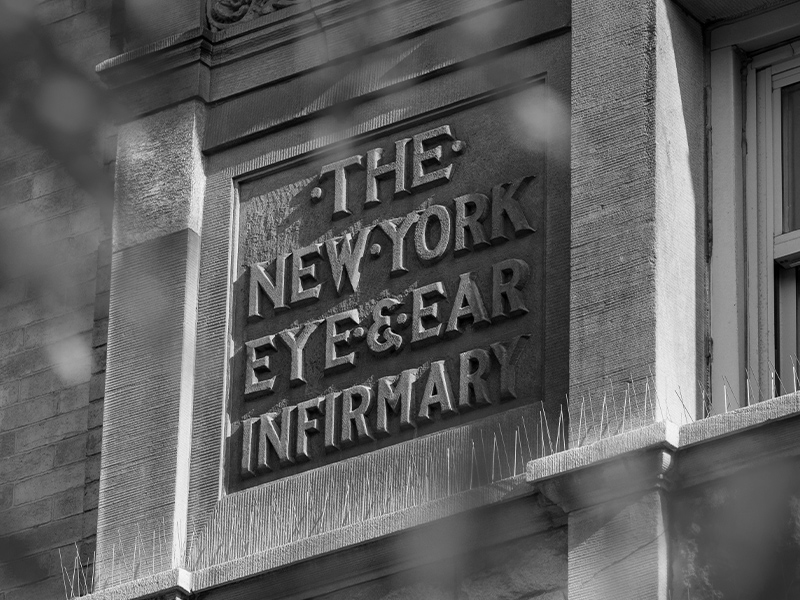
The history of New York Eye and Ear Infirmary of Mount Sinai (NYEE) began in 1816 when two young physicians from New York, Dr. Edward Delafield and Dr. John Kearny Rodgers, sailed to England to study at the London Dispensary for Curing Diseases of the Eye and Ear (known today as Moorfields Eye Hospital). Guided by their deep sense of social responsibility and inspired to translate their newfound medical insights into action, Drs. Delafield and Rodgers founded New York Eye Infirmary (later named New York Eye and Ear Infirmary), the first specialty hospital in America. From its humble beginnings as a charitable institution, NYEE has grown into one of the best specialty hospitals in America, a place where discoveries and innovations have helped to shape the fields of ophthalmology and otolaryngology and impact thousands of lives. This timeline represents a few of the highlights over our first 200 years.

1816
Drs. Edward Delafield and John Kearny Rodgers, recent graduates of the College of Physicians and Surgeons, leave for England to continue their education. They are introduced to lectures at the Royal London Ophthalmic Hospital.

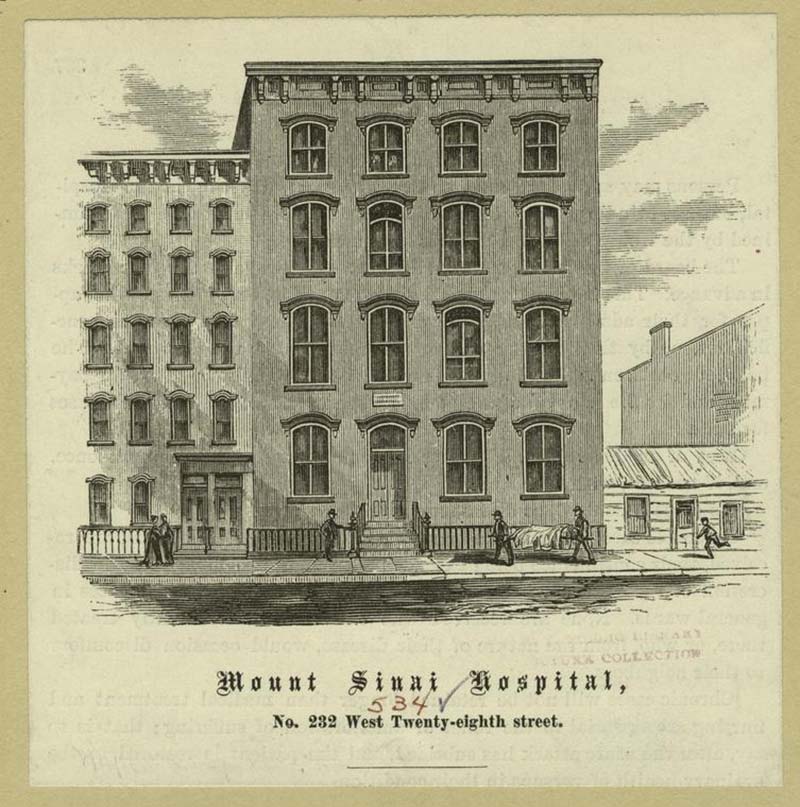
1820
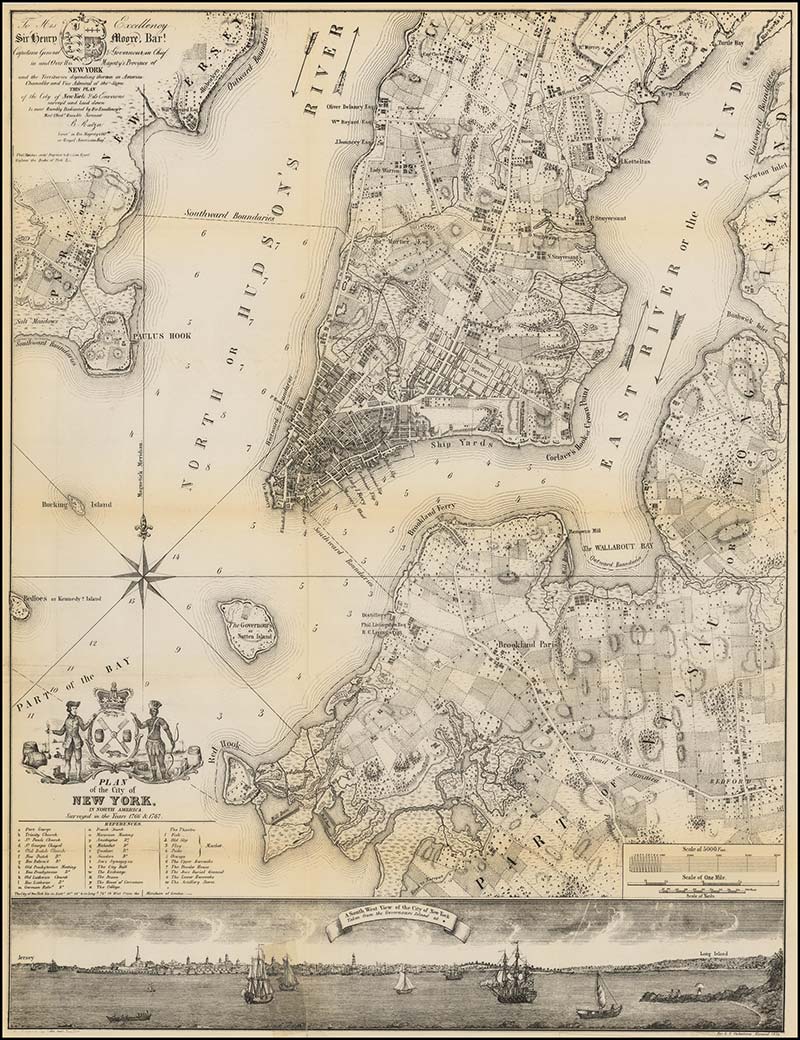
Drs. Edward Delafield and John Kearny Rodgers open the New York Eye Infirmary, the first specialty eye hospital in the Western Hemisphere, on August 14, 1820, located on 45 Chatham Square in New York City.
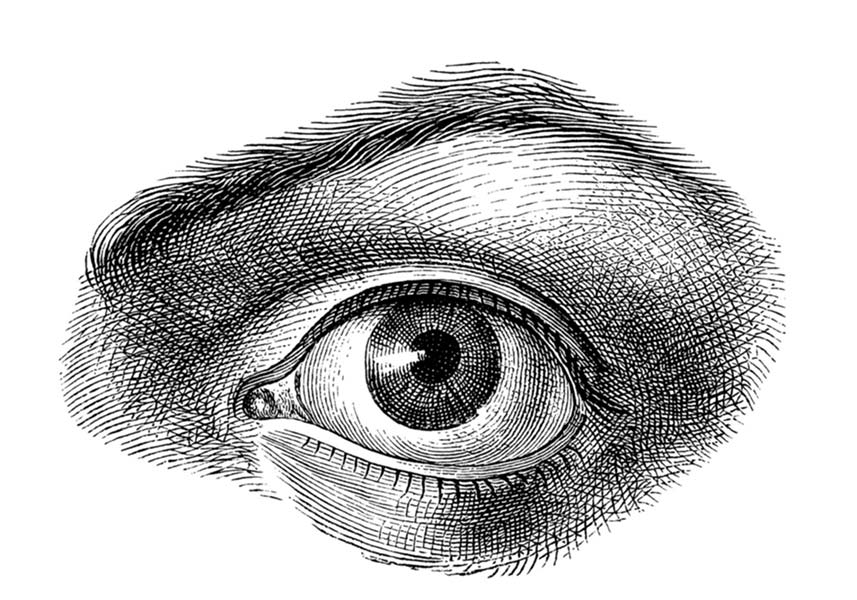
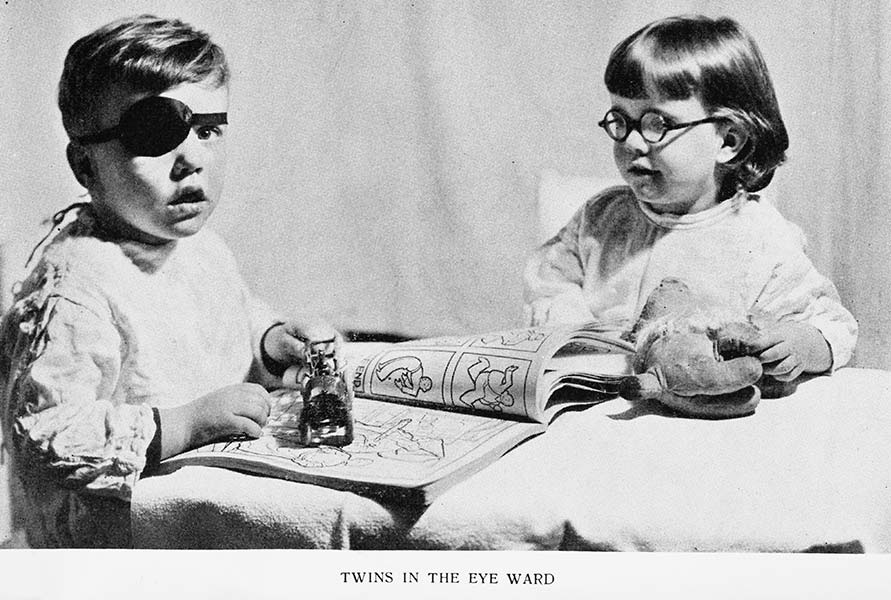
Infirmary surgeons perform the first successful congenital cataract surgeries in the United States restoring vision to three pediatric patients.
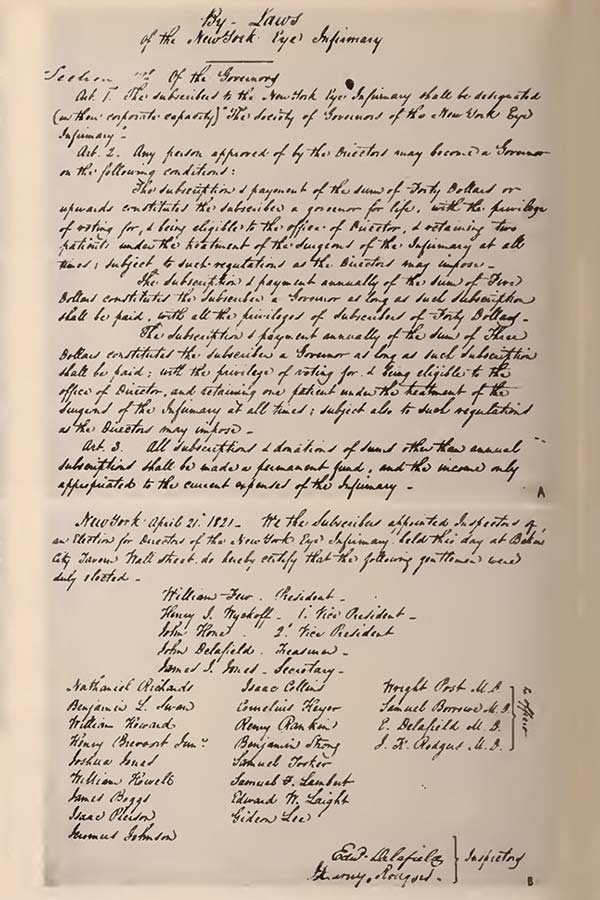
1821
The Society of the New York Eye Infirmary, a formal charity, is created with bylaws modeled after the U.S. Constitution at the suggestion of the Infirmary’s first president, Colonel William Few, one of the signers of the U.S. Constitution.
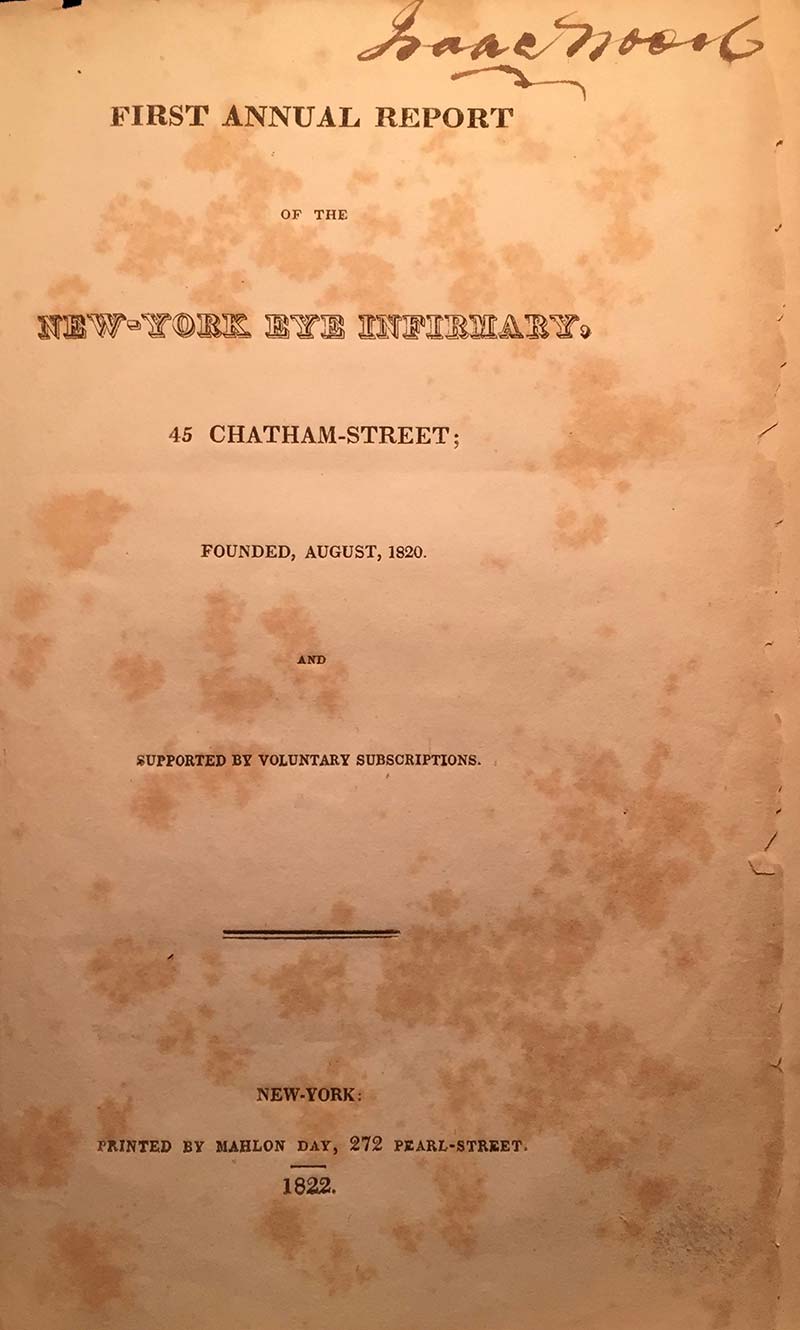
1822
The first New York Eye Infirmary Annual Report is published in the New York-American newspaper. The Report documents that in little more than a year, 1,120 persons afflicted with diseases of the eye had come forward for relief, 801 of whom were deemed cured.
1822
On March 22, 1822, the New York State Legislature formally recognizes the incorporation of the New York Eye Infirmary. As such, ophthalmology becomes the first specialty to be recognized by the medical profession and the legislature.
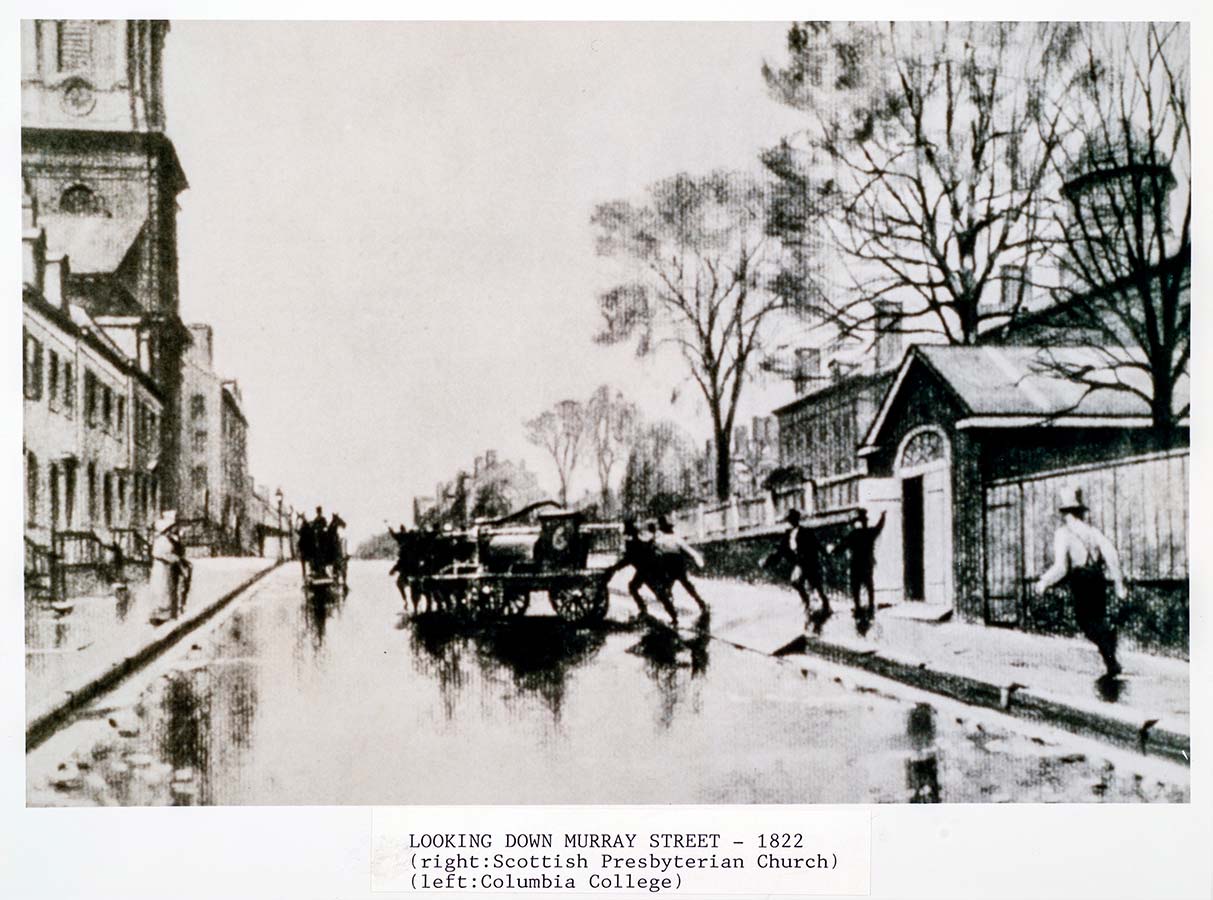
1822
The New York Eye Infirmary relocates to new quarters on Murray Street.
New York City’s yellow fever epidemic forces the Infirmary to shutter its doors for three months.
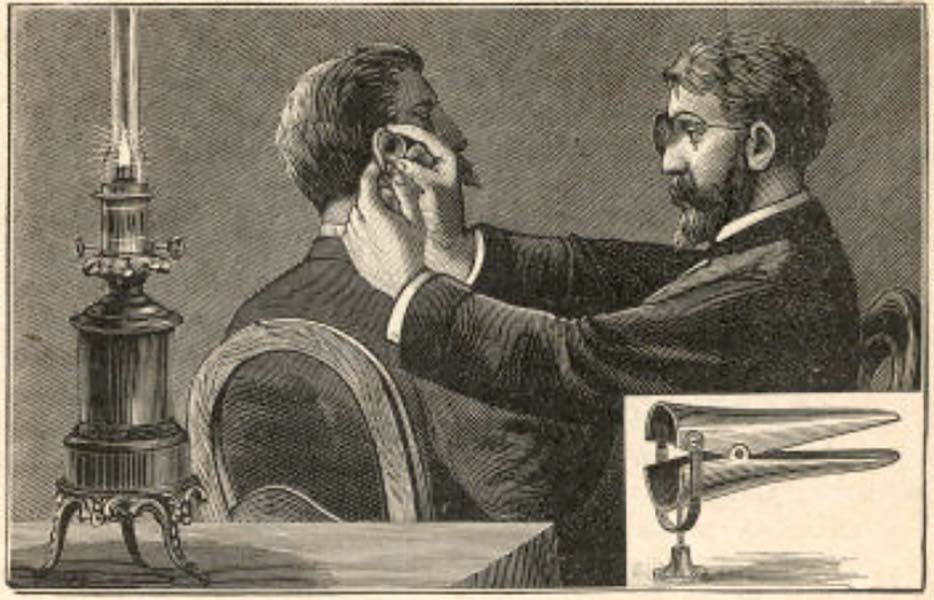
1822
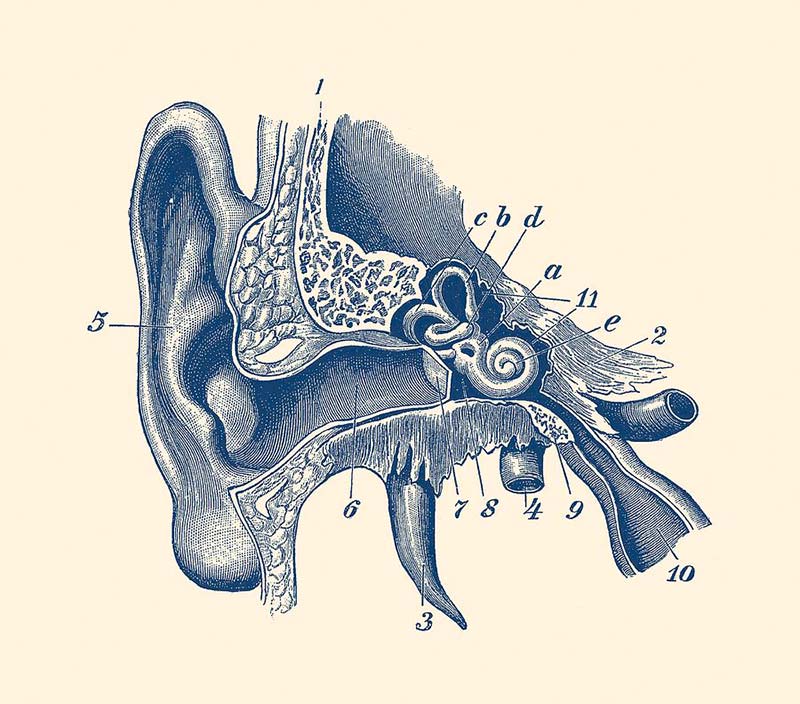
The New York Eye Infirmary adds its first “aurist” to its staff.
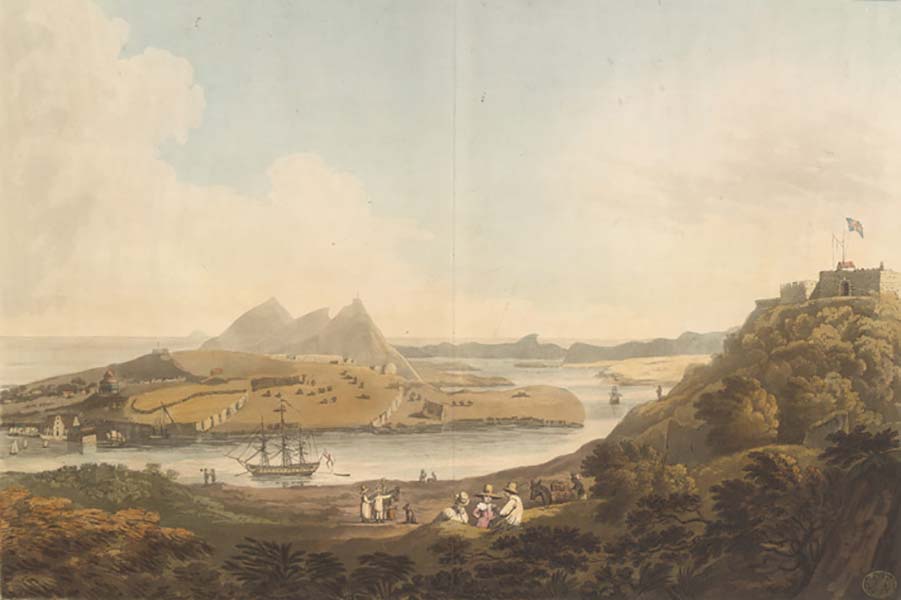
1823
Dr. Rodgers travels to Curaçao, West Indies, at the request of the island’s Rear Admiral Governor, to perform surgery in what might be called ophthalmology’s first international good will mission.
1824
Dr. Delafield introduces the first formal lectures in ophthalmology for medical students attending the College of Physicians and Surgeons.
1824
The New York Eye and Ear Infirmary establishes the first Otology Service in New York City and the first in the U.S.
1824
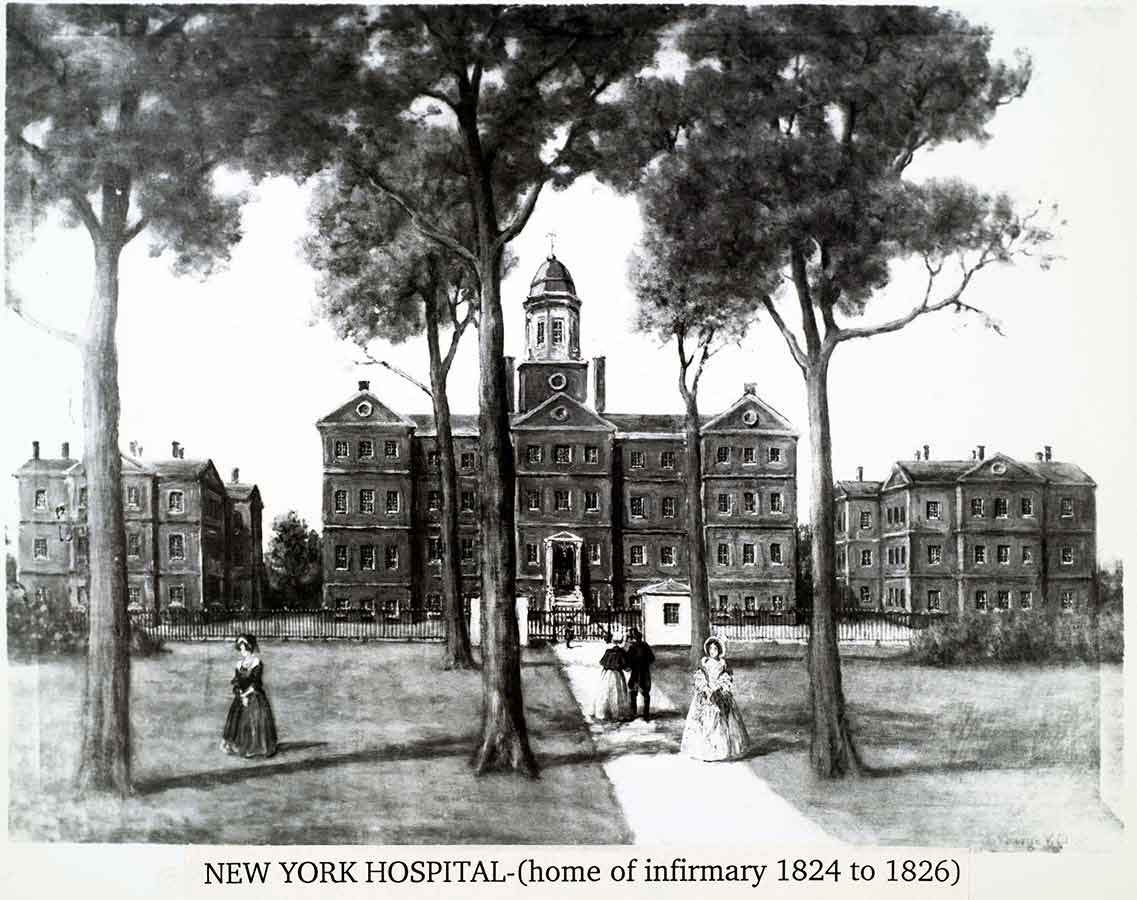
The New York Eye Infirmary relocates to its third home inside the Old Marine Hospital, at 139 Duane Street on the New York Hospital campus.
1824
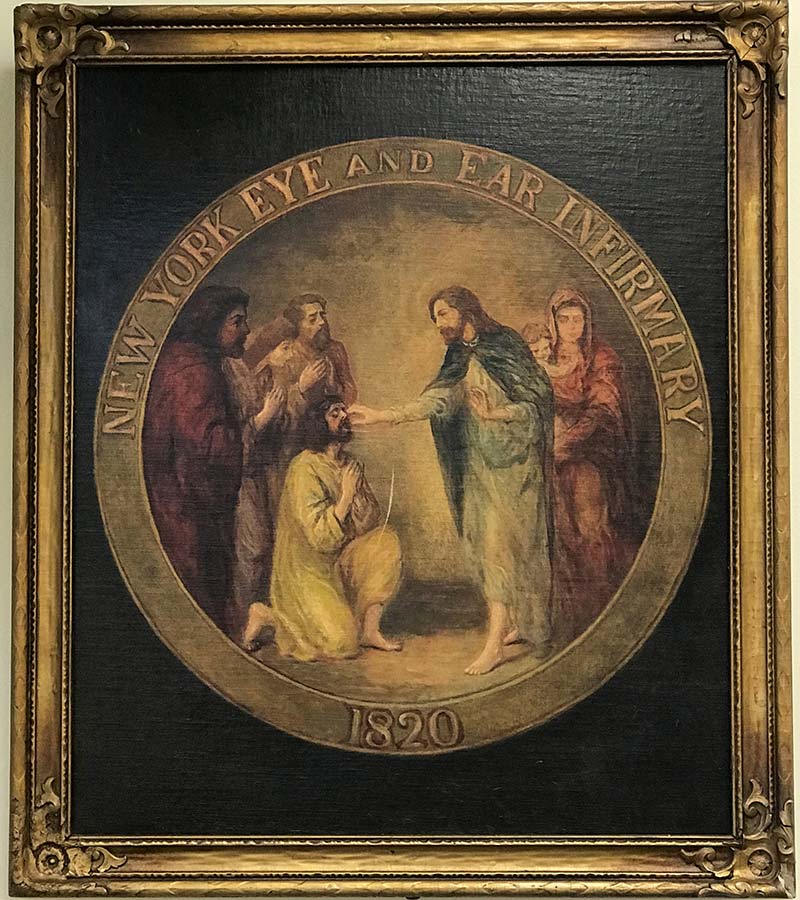
The Infirmary creates its original seal depicting the Great Physician restoring the sight of Bartimaeus. The American Ophthalmological Society adopts the Infirmary’s seal as its own upon its founding forty years later within the institution.
1827
In 1827, the New York Eye Infirmary relocates to its fourth home at 459 Broadway.
In 1834, the New York Eye Infirmary relocates to its fifth home at 96 Elm Street.
In 1840, the New York Eye Infirmary relocates to its sixth home at 45-47 Howard Street.
In 1845, the New York Eye Infirmary relocates to its seventh home at 97 Mercer Street.
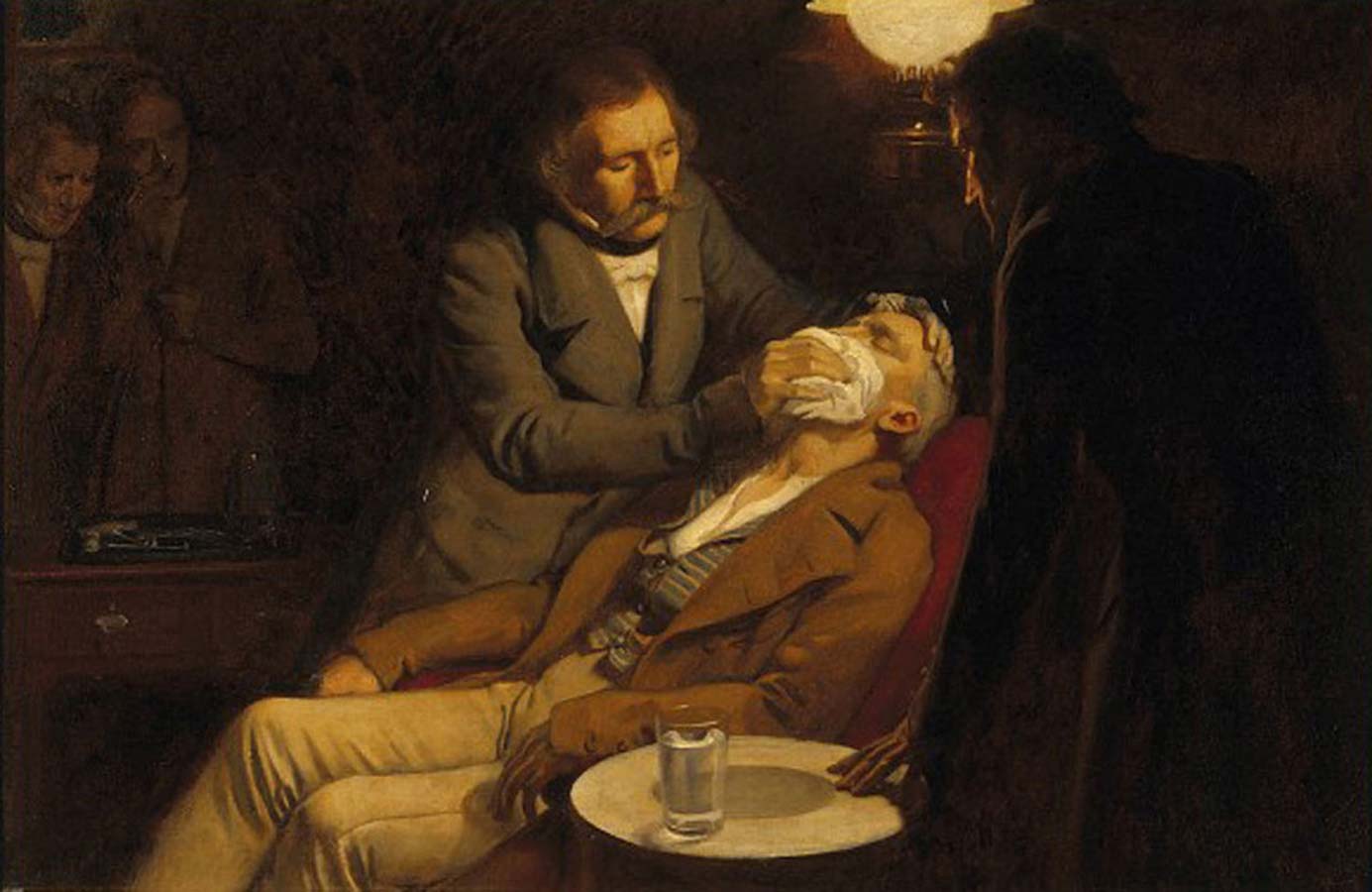
1846
Dr. William T. G. Morton demonstrates the use of ether-induced anesthesia at Massachusetts General Hospital in Boston to remove a jaw tumor, revolutionizing the field of surgery.
Thirty-one days later, Dr. Rodgers uses ether in a procedure to drain a perirectal abscess at the New York Hospital.

1848
Dr. Rodgers is one of the first surgeons in New York City to ligate the innominate artery.

1850
Dr. David Kearny McDonogh, America’s first African-American ophthalmologist, adopts Dr. John Kearny Rodger’s middle name in honor of his mentor under whom he practiced for 11 years.

1851
The New York Eye Infirmary’s Dr. Gurdon Buck, the “father of intralaryngeal surgery,” develops a method of laryngofissure to treat laryngeal carcinoma, as well as a technique to reduce edema of the glottis before the invention of the laryngoscope. He is also known for his contributions to orthopedic traction (Buck’s extension) and genitourinary tract anatomy. Buck’s fascia is named after him.
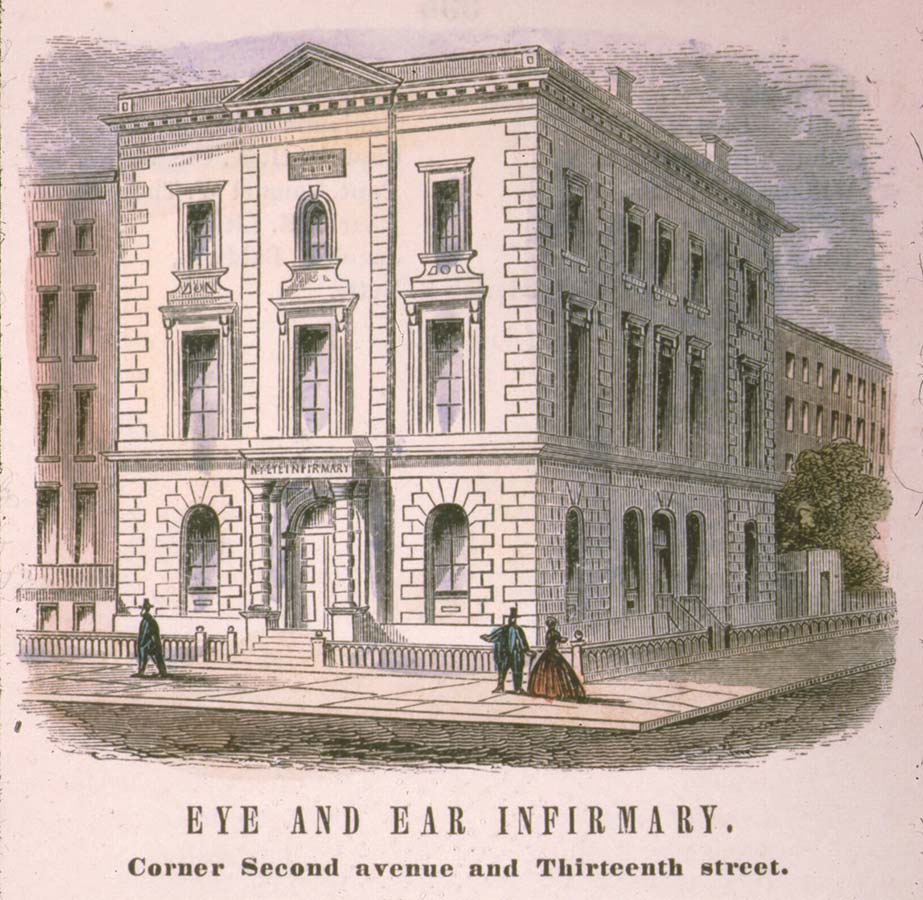
1856
The New York Eye Infirmary moves to its eighth and permanent home, at Second Avenue and East 13th Street, on April 25.
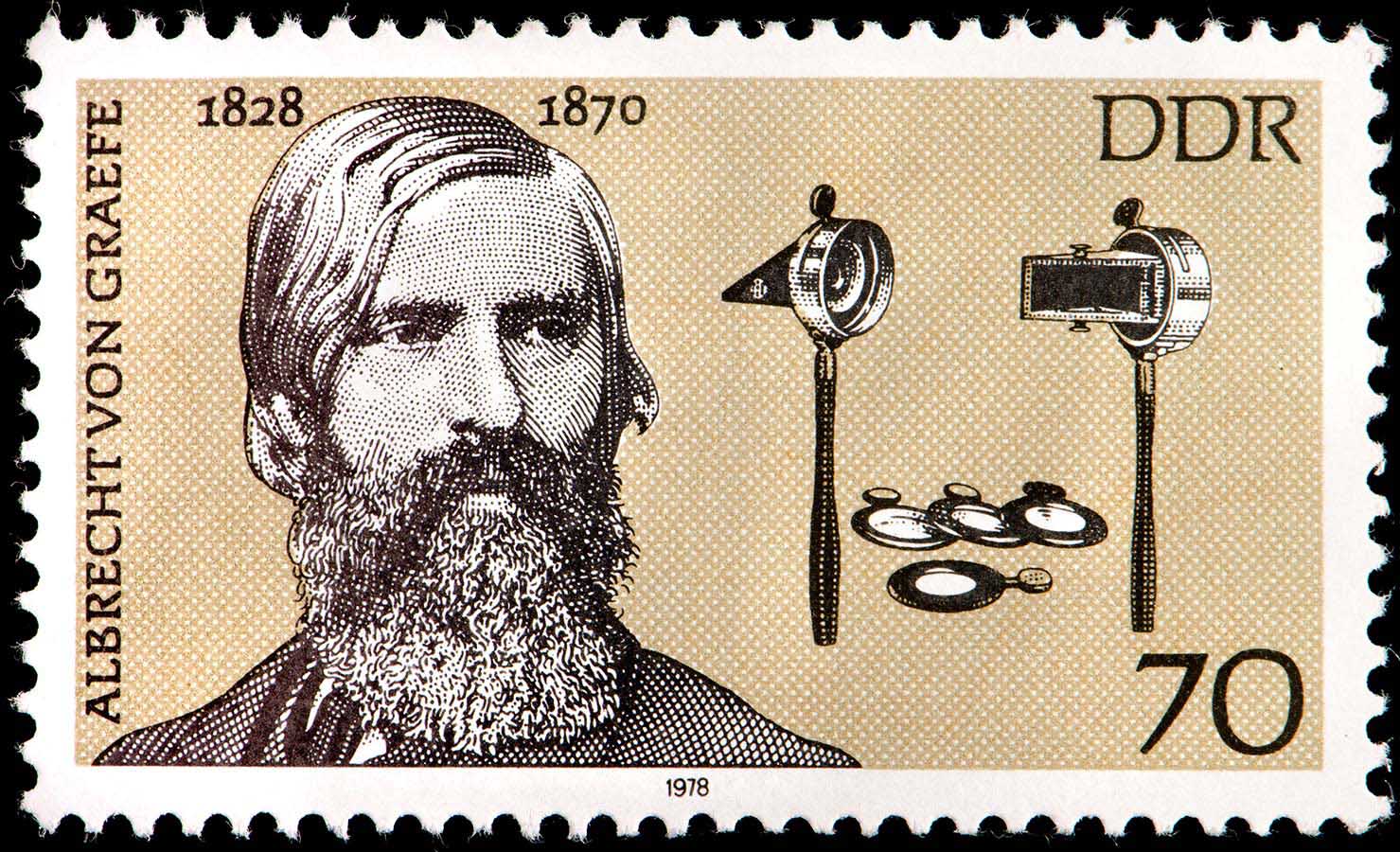
1858
Drs. Cornelius Agnew and Henry D. Noyes, two New York Eye Infirmary graduates, return home to New York after studying under Dr. Albrecht von Graefe, and initiate lectures about and demonstrations of the medical advances and state-of-the-art instrumentation practiced in Europe.
1862
Dr. Noyes, now Executive Director of the New York Eye Infirmary, is the first to photograph the retina of a living creature, a rabbit, laying the foundation for modern clinical retinal imaging.
The New York Eye Infirmary appoints its first house surgeon.

1862
Dr. William T. G. Morton (who first publicly demonstrated the use of inhaled ether as a surgical anesthetic in 1846) sues New York Eye Infirmary for patent infringement and loses. The verdict establishes the landmark “patentability of a principle of nature” decision, freeing the medical profession to employ ether anesthesia without prejudice.
1864
Drs. Noyes and Agnew, with several of their colleagues from around the city, found the New York Ophthalmological Society, the first specialty medical society in the U.S., and meet on March 7.
1864
An Act of the New York State Legislature officially changes the name of The New York Eye Infirmary to The New York Eye and Ear Infirmary, in formal recognition of its Otology Service, first established in 1824.
1864
The American Ophthalmological Society (AOS), the second oldest specialty medical society in the United States, is founded on June 7 by Drs. Noyes and Hasket Derby of Boston. They invite 16 of their esteemed colleagues to join and name Dr. Delafield as the AOS’s first president. The organization’s first two annual meetings are held at the Infirmary.
1866
Dr. Cornelius Agnew founds the Clinic for the Diseases of the Eye and Ear at Columbia University's Vagelos College of Physicians and Surgeons.
1868
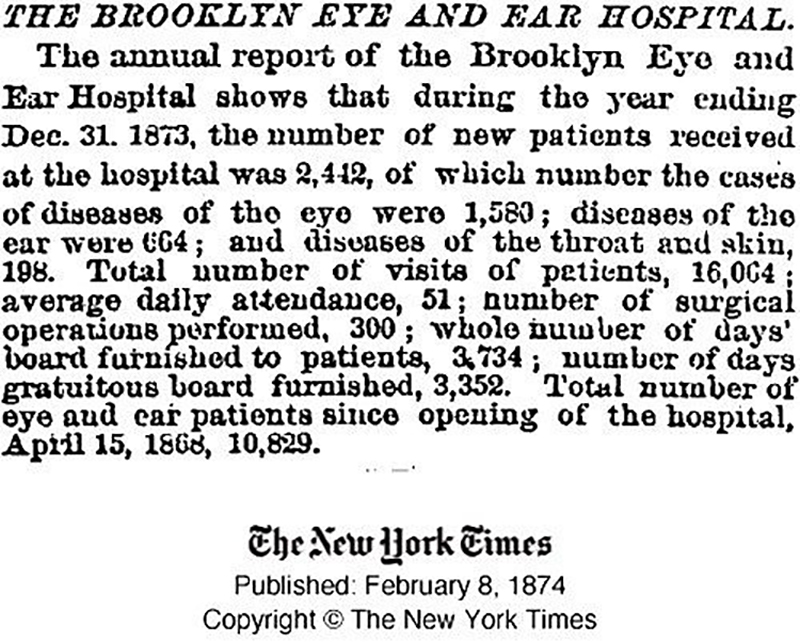
Dr. Agnew helps to found the Brooklyn Eye and Ear Hospital.

1868
At a meeting of the American Ophthalmological Society, Dr. Noyes, along with eight other members of that Society, propose the formation of the American Otological Society and compose its bylaws and constitution.
1869
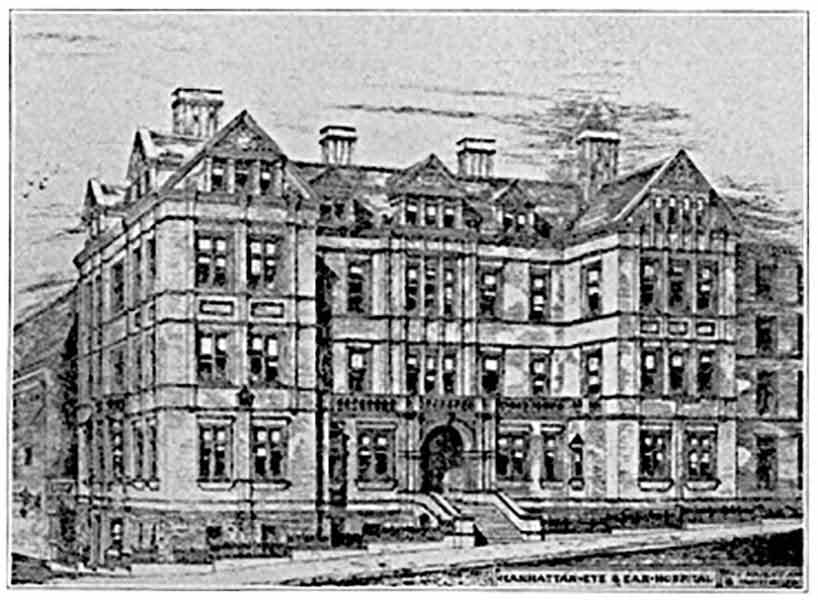
Dr. Agnew is among the founders of the Manhattan Eye, Ear and Throat Hospital.
1871
Dr. Agnew invents a new incision for draining the lacrimal sac made through the conjunctiva between the caruncle and the inner commissure of the eyelids.
1873
The NYEE Throat Department is established as the forerunner of the Head and Neck Service.
1873
NYEE physicians help found The New York Laryngological Society, the first of its kind in the United States and a precursor to the American Laryngological Society, established in 1878.
1874
NYEE surgeons begin to chart detailed accounts of their cases as was already customary in Europe.
1878
Dr. Emil Gruening joins NYEE staff where he becomes a Surgeon Director.

1878
NYEE expands with the opening of the Green Pavilion.
NYEE initiates its first voluntary 10-cent charge for prescriptions.

1884
Quarantine of Contagious Ophthalmia Cases

1885
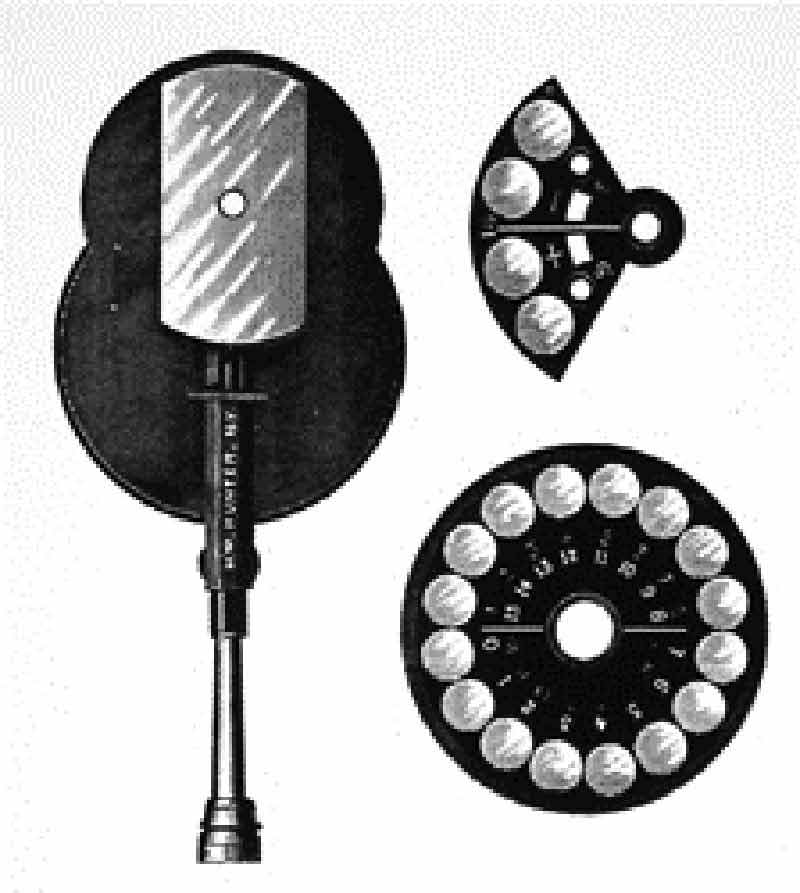
Dr. William Dennett, a NYEE attending, invented first Ophthalmoscope with illuminating light bulb.
1885
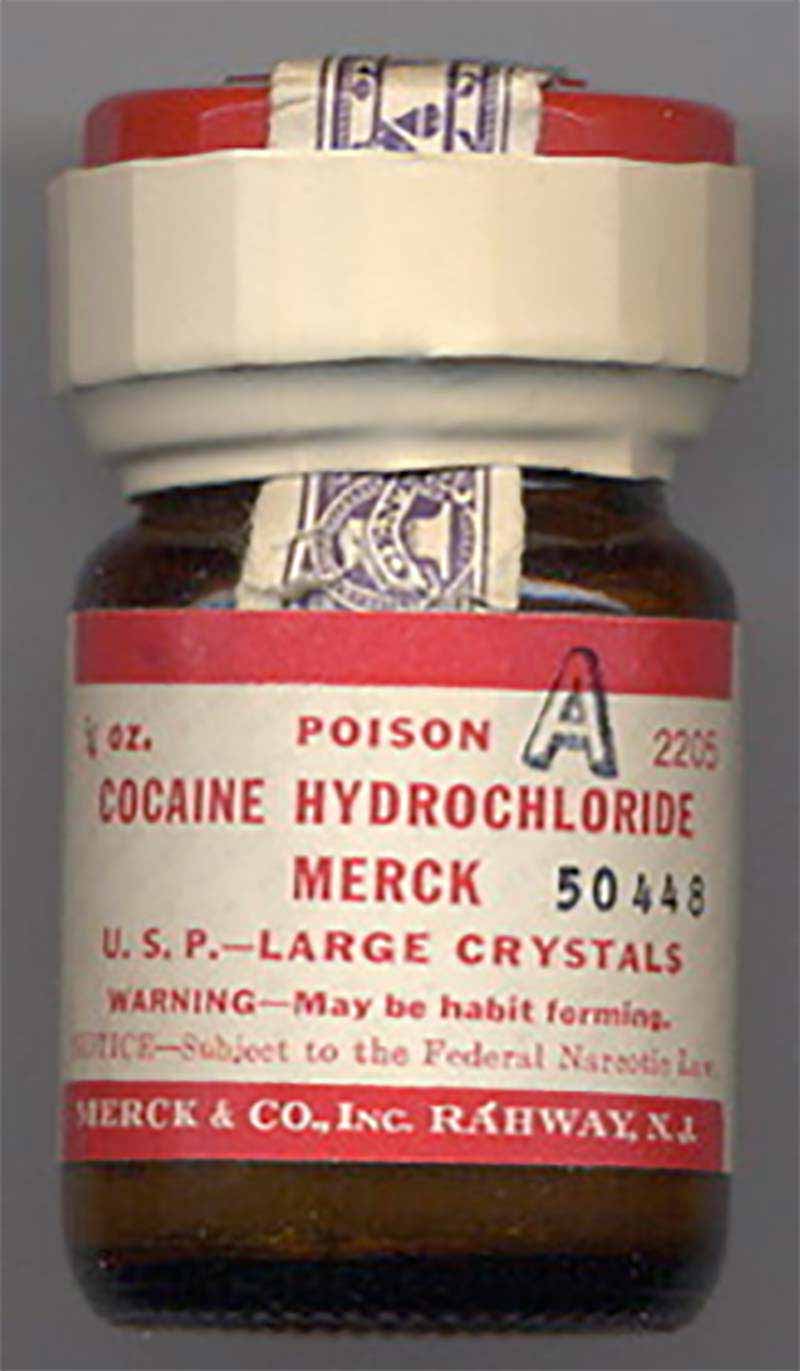
Dr. Carl Koller comes to NYEE to demonstrate cocaine anesthesia for ocular surgery.
1886
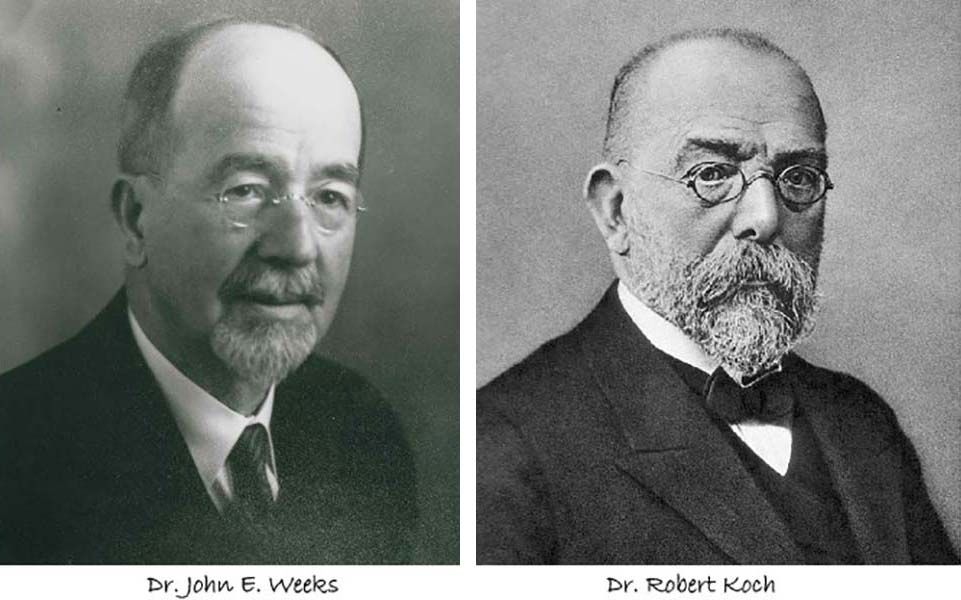
Haemophilus aegyptius or Koch‐Weeks bacillus is discovered by Drs. Robert Koch and John E. Weeks, head of the NYEE staff, as a cause of acute conjunctivitis.
1886
Dr. Agnew details a groundbreaking operation for divergent strabismus, in an article entitled "A Method of Operating for Divergent Squint," published in the Transactions of the American Ophthalmological Society.
1886
Dr. Francis Delafield, noted pathologist and son of Dr. Edward Delafield, is elected the first president of the Association of American Physicians. Dr. Delafield also mentors Dr. William Welch, founder of Johns Hopkins Medical School.
1888
Dr. Edward G. Loring enhances the Helmholtz Ophthalmoscope with design features to improve ergonomics for the clinician.
1888
NYEE's Executive Surgeon Dr. Noyes publishes his groundbreaking Textbook on the Diseases of the Eye.
1888
Dr. Koller joins the NYEE staff. Subsequently, he becomes a member of The Mount Sinai Hospital’s staff and is named Chief of the Eye Clinic.
1888
Radical mastoid drainage surgery is introduced to the United States by Dr. Emil Gruening at The Mount Sinai Hospital.
1890
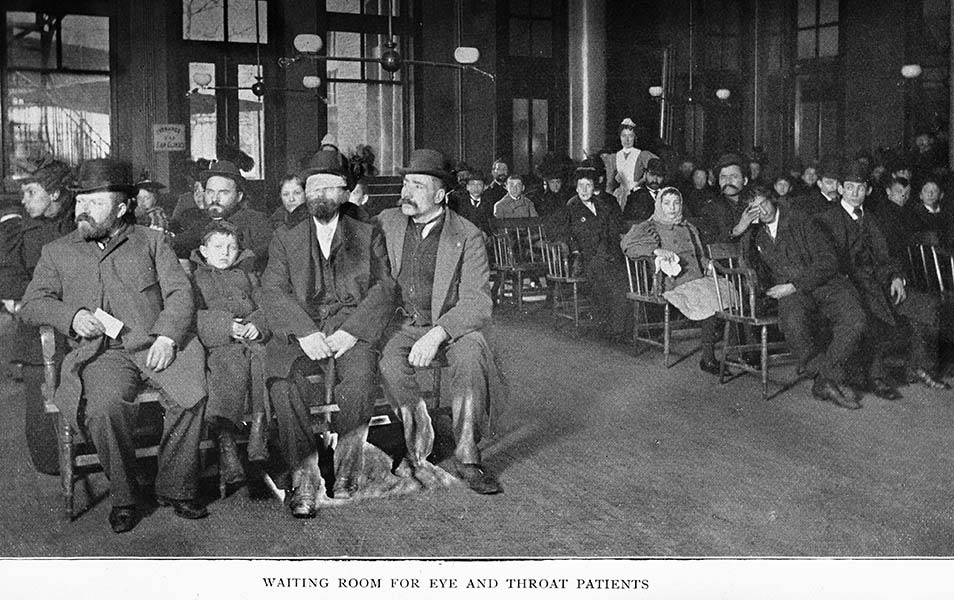
NYEE hosts a cornerstone-laying ceremony to celebrate its next major expansion.
New York Eye and Ear Infirmary School of Ophthalmology and Otolaryngology, after seven decades of lectures and clinical training, is officially recognized and chartered by the New York State Legislature.
1890
Dr. Gruening organizes the Ear, Nose, and Throat Clinic at The Mount Sinai Hospital.
1892
The New York Otologic Society is founded by several physicians, including NYEE’s Dr. Edward Dench, Surgeon Director.
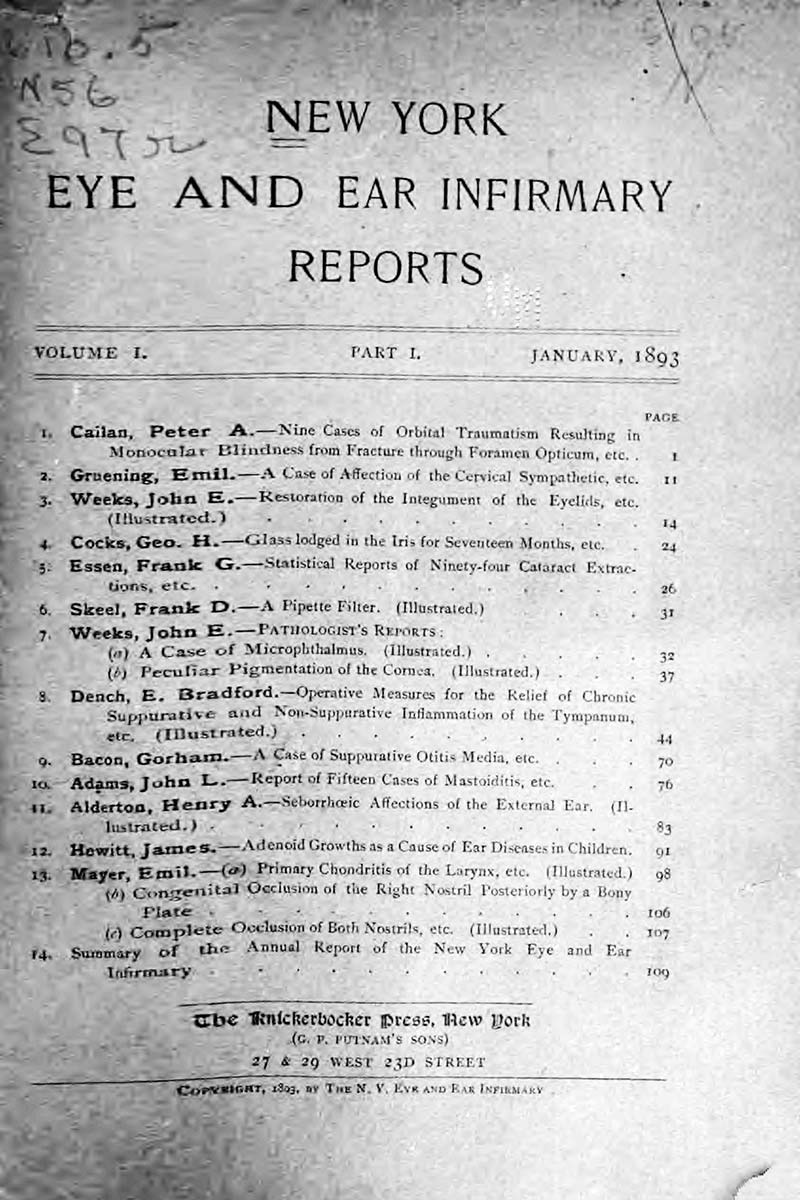
1893
NYEE publishes the first edition of The New York Eye and Ear Infirmary Reports.
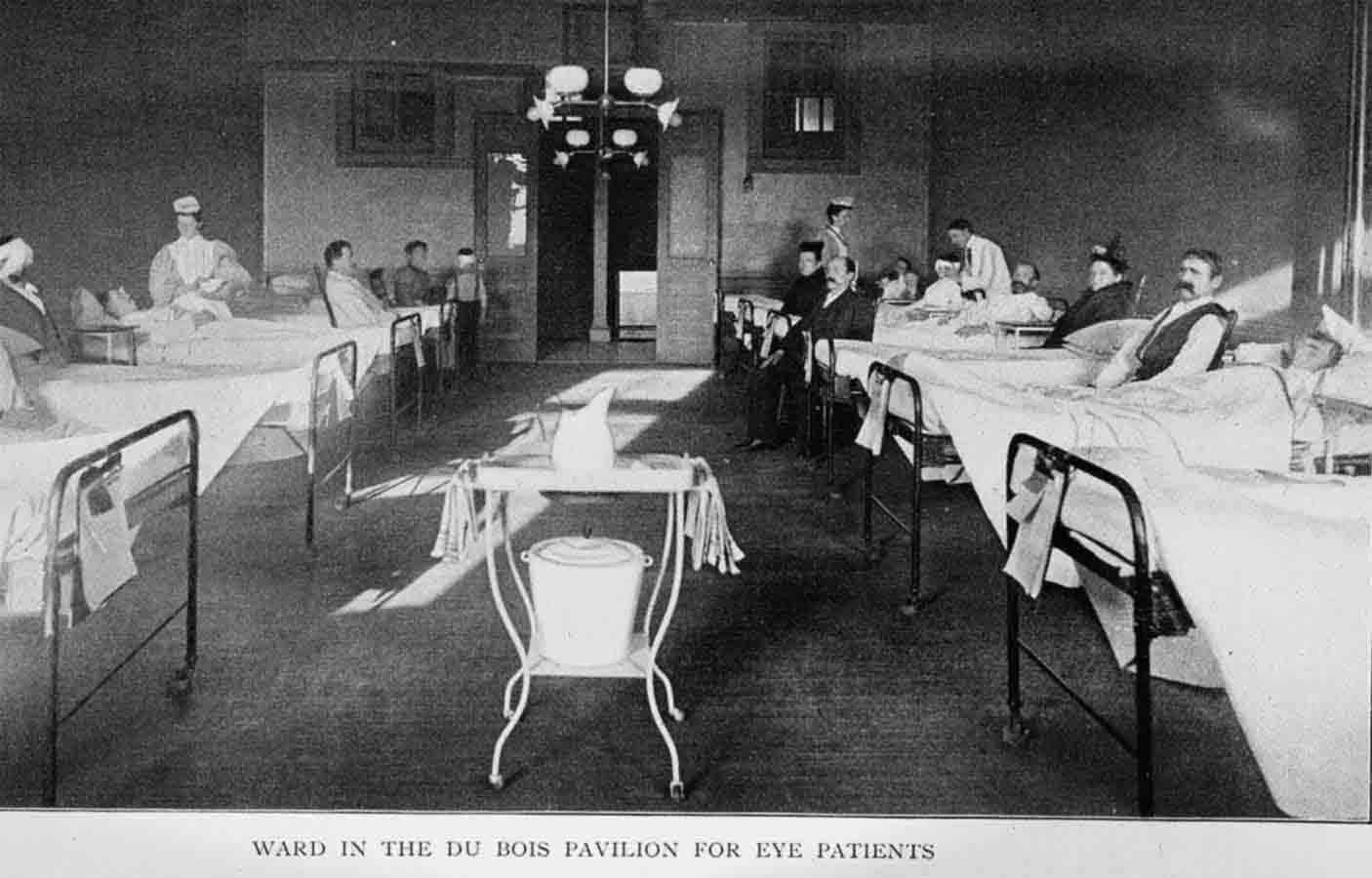
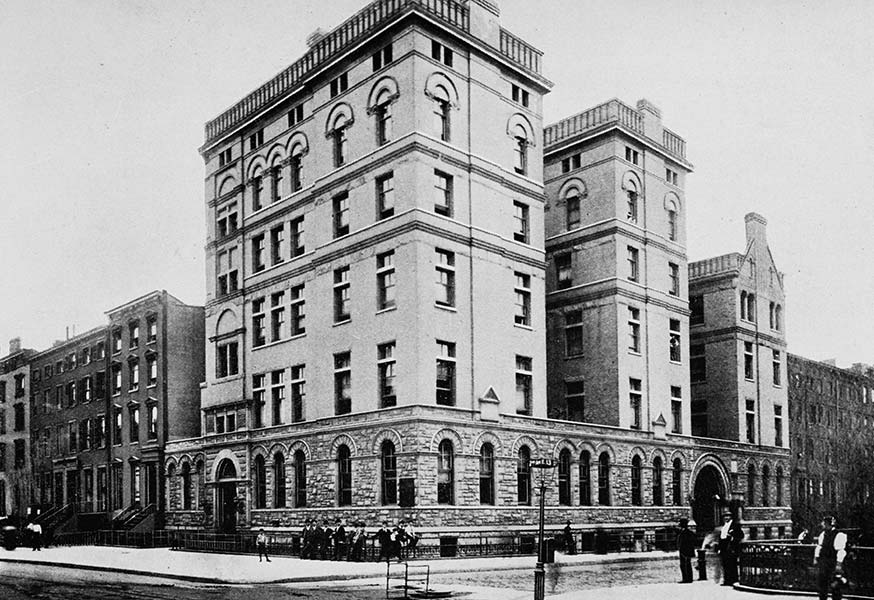
1894
NYEE opens its five-story building and the Abram Du Bois Pavilion on Second Avenue and East 13th Street.
1896
NYEE separates its Ophthalmology and Otolaryngology services.

1899
The New York Eye and Ear Infirmary Post-Graduate School for Nurses is created by the NYEE’s Board of Directors.
1901
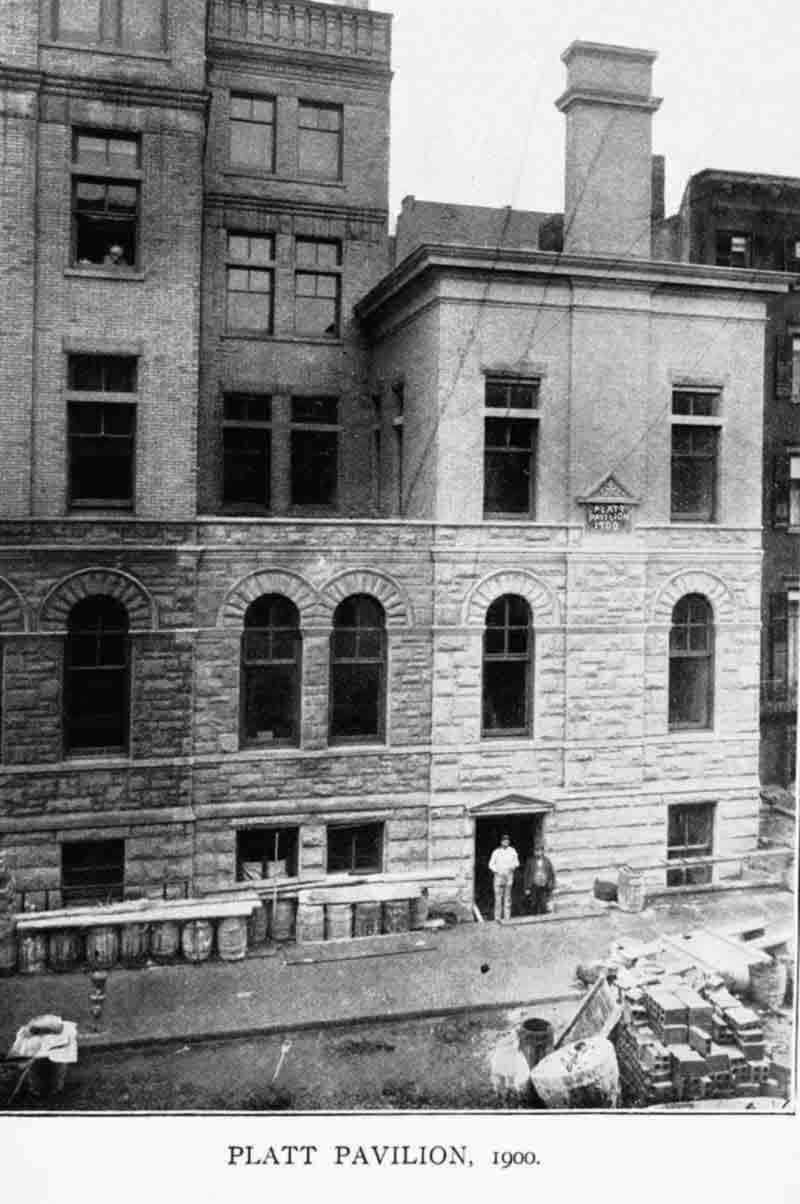
NYEE opens the James N. Platt Pavilion for the treatment of contagious eye diseases.

1903
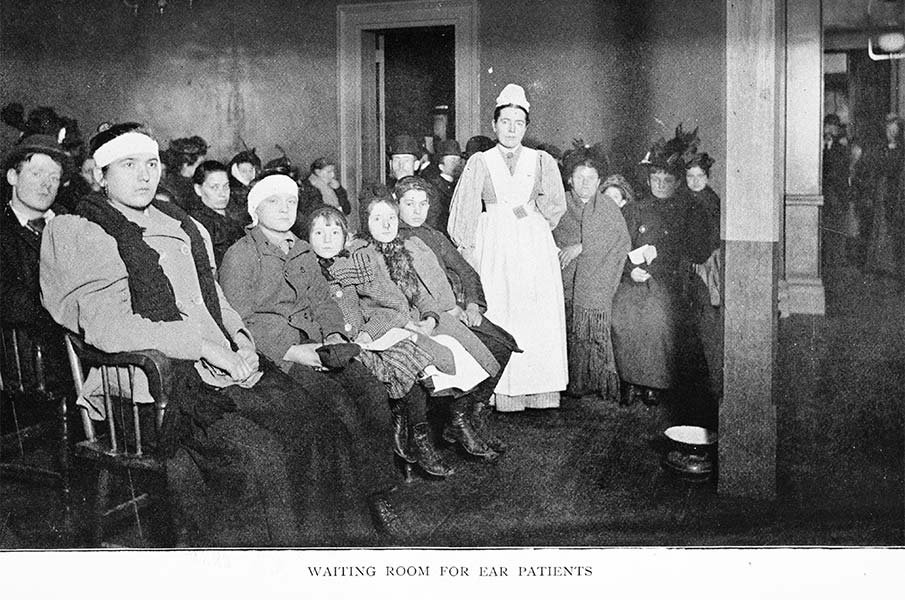
Helen Keller is a guest of honor and speaks at the Infirmary’s dedication of the William C. Schermerhorn Pavilion for the treatment of ear diseases.
1903
NYEE initiates its first voluntary 25-cent charge for clinic visits. A fee that will last for the next fifty years.
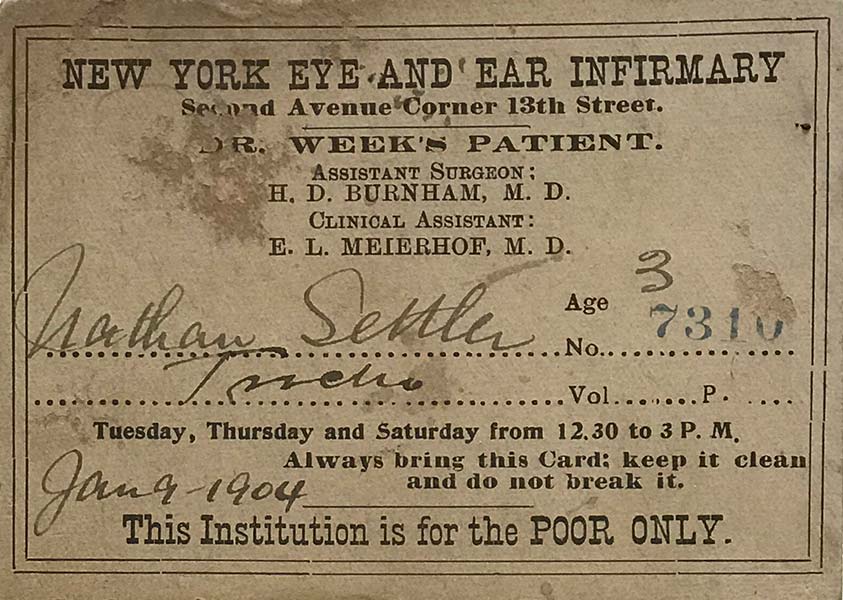
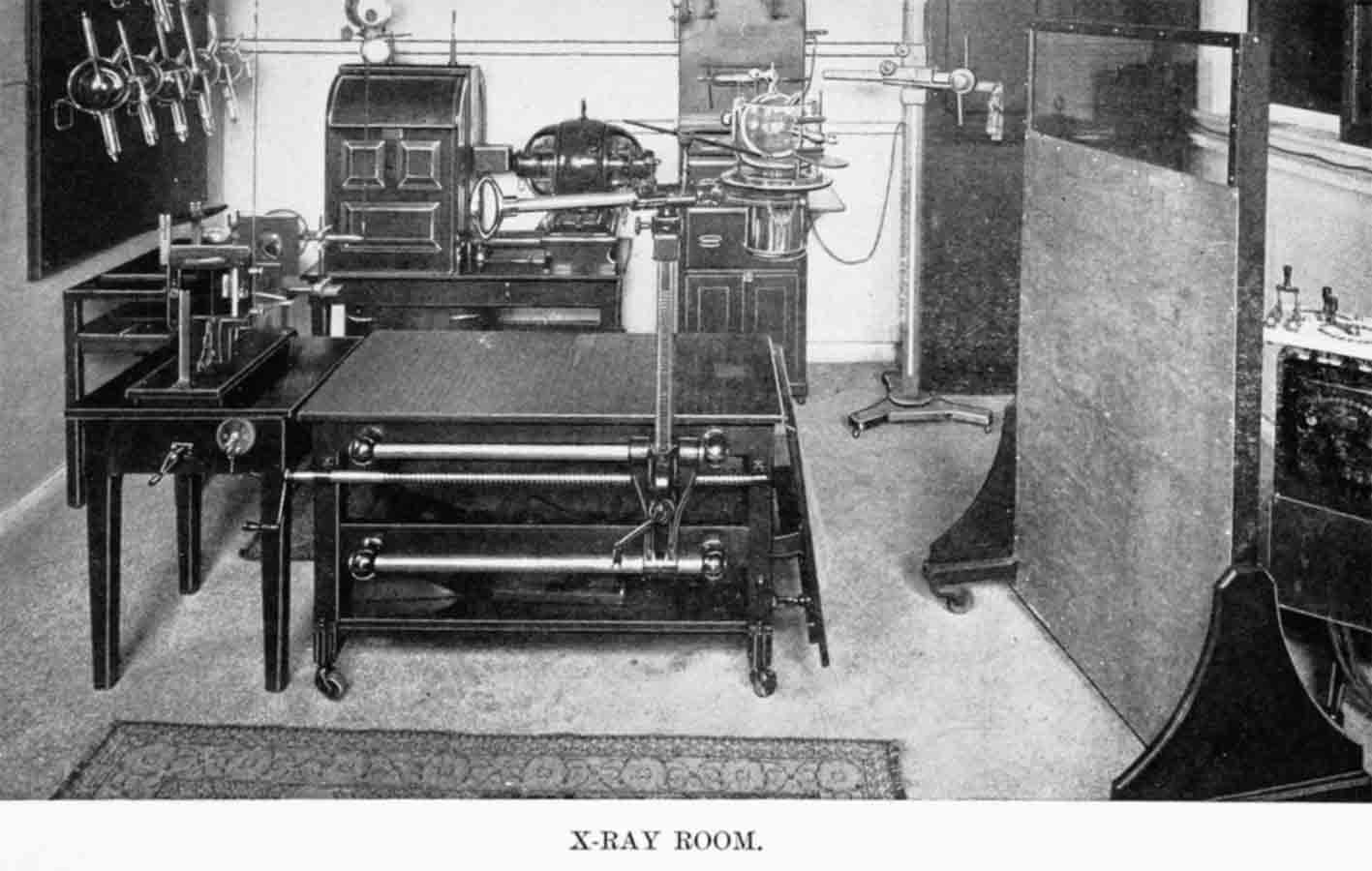
1904
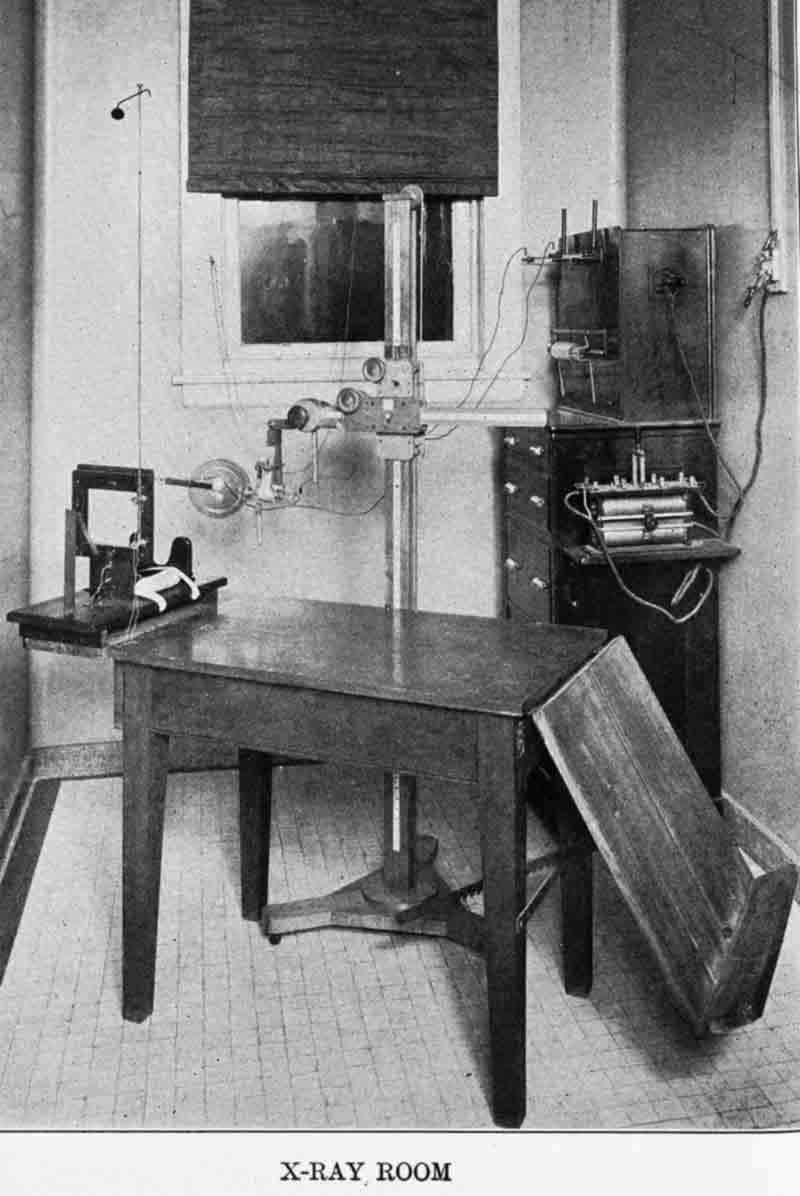
In 1904, NYEE’s first X-ray Department is established by Dr. Weeks with the purchase of the Infirmary’s first X-ray equipment.
The first x-ray localization of a foreign body in a patient’s eye is performed by Drs. Weeks and George Dixon. Subsequently, Dr. Dixon develops the Weeks and Dixon method of ocular foreign body localization.
In 1905, Dr. Weeks donates his X-ray apparatus to the Infirmary.
1910
NYEE upgrades its radiology department with new X-ray technology donated by the Hartley-Jenkins family.

1910
Dr. F. Phinzy Calhoun, NYEE resident class of 1908, returns to Atlanta to develop and lead the department of ophthalmology at Grady Hospital and Emory University for the next 30 years.

1911
Dr. Harvey J. Howard, NYEE resident class of 1910, is recruited to head the Department of Ophthalmology at the University Medical School, Canton, China, and subsequently becomes ophthalmologist to the child emperor Puyi, the last Emperor of China. Eventually, he establishes the Department of Ophthalmology at Washington University in 1928.

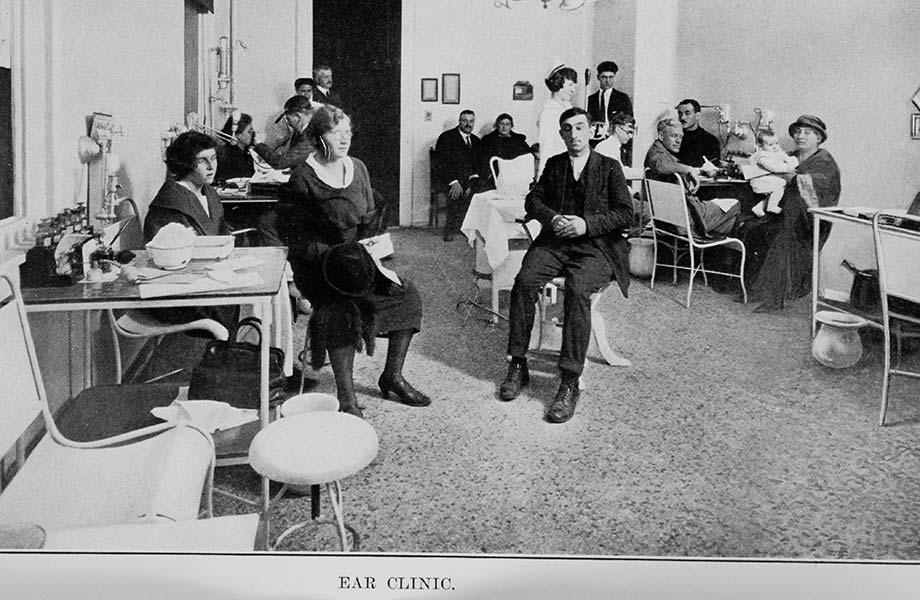
1915
NYEE's Social Services Department is established under the direction of Florence M. Campbell.
1915
NYEE expands its footprint to East 14th Street with the acquisition of contiguous lots 310, 312, and 314 and, shortly thereafter, lot 308.

1919
NYEE becomes part of the New York United Hospital Fund charitable trust.
1919
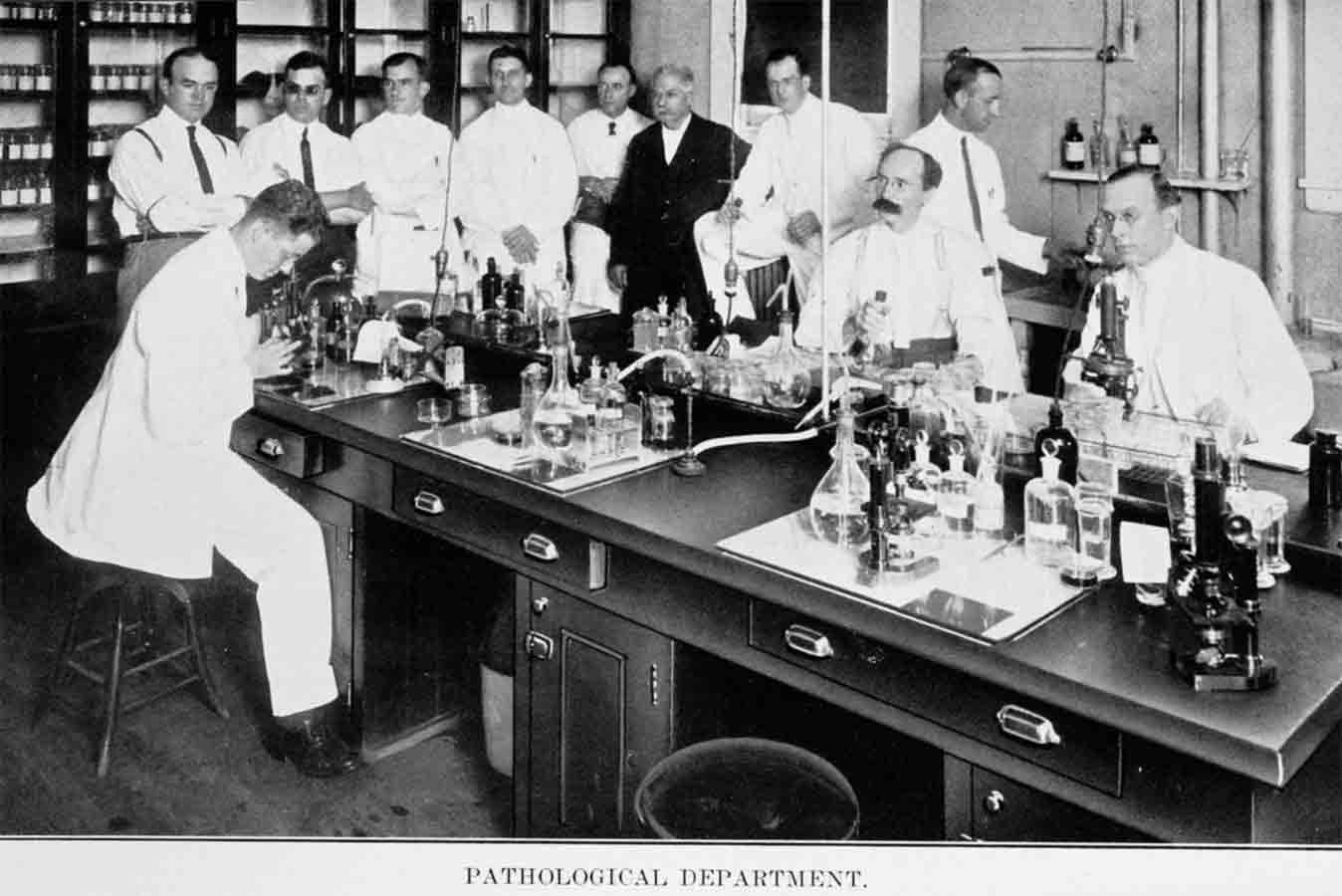
In 1919, Dr. Bernard Samuels, NYEE resident, takes charge of NYEE's Pathology Department. At the end of his career, in 1957, Dr. Samuels, with the aid of the Board of Surgeons and Directors of the New York Eye and Ear Infirmary and supported by Dr. Moacyr Alvaro of Sâo Paulo, Brazil, Executive Director and past President of the Pan American Association of Ophthalmology, established the Institute of Ophthalmology of the Americas. The Institute was a post graduate teaching division of NYEE for Latin American Ophthalmologists and included a course for students of pediatric ophthalmology and strabismus.

1925
NYEE's Social Service Department comes under the direction of the Auxiliary Social Service Committee.

1926
NYEE's Department of Research is created by Dr. Conrad Berens, NYEE resident class of 1915.

1928
Dr. Conrad Berens establishes the Association for Research in Vision and Ophthalmology (ARVO). The Association was originally called the Association for Research in Ophthalmology (ARO). Today, ARVO is the largest and most respected eye and vision research organization in the world with international membership of nearly 11,000 researchers from over 75 countries.

1933
Dr. John Martin Wheeler, NYEE resident class of 1910, is chosen as the first director of the newly established Edward S. Harkness Eye Institute at Columbia University; he recruits his staff largely from the New York Eye and Ear Infirmary.
1933
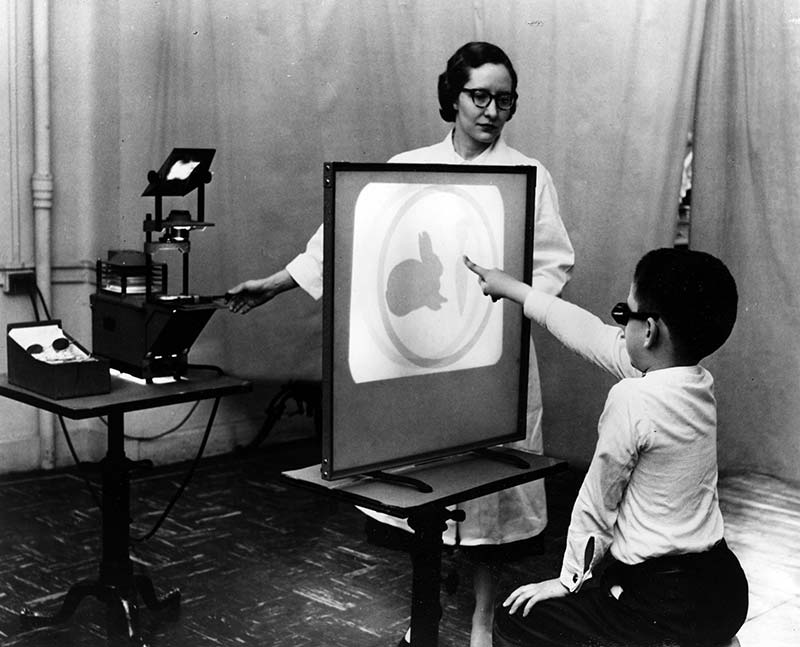
Dr. Berens established an Orthoptic Clinic at New York Eye and Ear Infirmary.

1934
Dr. Wheeler pioneers the specialty of ophthalmic plastic and reconstructive surgery with the new techniques for the repair of eyelid abnormalities, including lower eyelid entropion, which is still in use today. He also introduces the first oculoplastic courses at the American Academy of Ophthalmology.

1934
NYEE acquires New York City’s first eikonometer.

1935
NYEE establishes the first School of Orthoptics in the U.S. under the direction of Dr. Berens and orthoptists Elizabeth K. Stark and Ethel Mueser.

1936
The American Academy of Ophthalmology and Otolaryngology selects NYEE as the site of its annual otolaryngologic section meeting.
1938
NYEE formalizes an academic affiliation with Columbia University College of Physicians and Surgeons, enabling NYEE house officers to participate in basic science courses at Columbia Presbyterian Hospital.

1938
NYEE surgeon Dr. Isaac Hartshorne develops a low cost portable binocular gonioscope.

1939
NYEE is asked to establish professional guidelines for orthoptic technicians and hosts the first national certifying examination of orthoptists.
1939
NYEE's Chief of Ophthalmic Plastic and Reconstructive Surgery, Dr. Wendell Hughes, develops the “Hughes Procedure” for reconstructing lower eyelid defects following the removal of large tumors. He is later honored by the American Society of Ophthalmic Plastic and Reconstructive Surgery with the establishment of the prestigious Wendell Hughes Lectureship.

1939
Dr. Berens introduces thermoplastic prism bars for measurement of strabismic deviation, replacing heavy and expensive glass prism bars.
1939
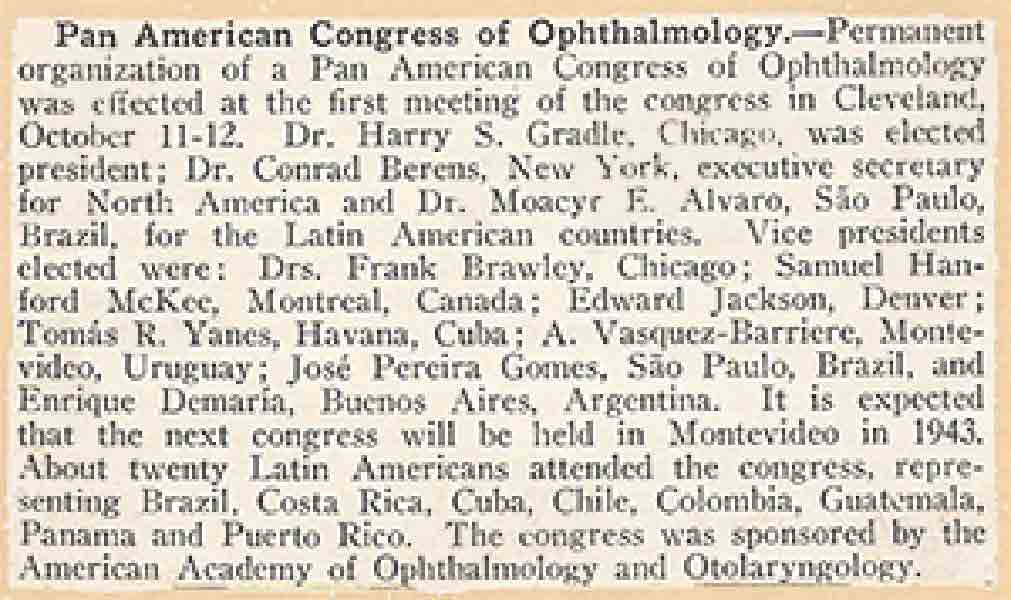
NYEE's Dr. Berens, along with Drs. Harry S. Gradle of Chicago and Moacyr E. Alvaro of São Paulo, Brazil, create a new international organization in the Americas aimed at promoting exchange of scientific information and ideas to develop programs to restore eyesight. Named The Pan-American Association of Ophthalmology (PAAO), the first educational meeting was held on October 10-12, 1940 in Cleveland, Ohio, co-sponsored by the AAO&O.
1941
NYEE is accredited by the American College of Surgeons.

1943
With 132 NYEE staff physicians serving in the U.S. Armed Forces, resulting in severe staff shortages, the Infirmary’s entire teaching program is temporarily placed under the guidance of Columbia University’s College of Physicians and Surgeons.
1944
Department of Audiology and Hearing Research is established at NYEE to care for returning World War II GIs experiencing service-related hearing deficits.
1944
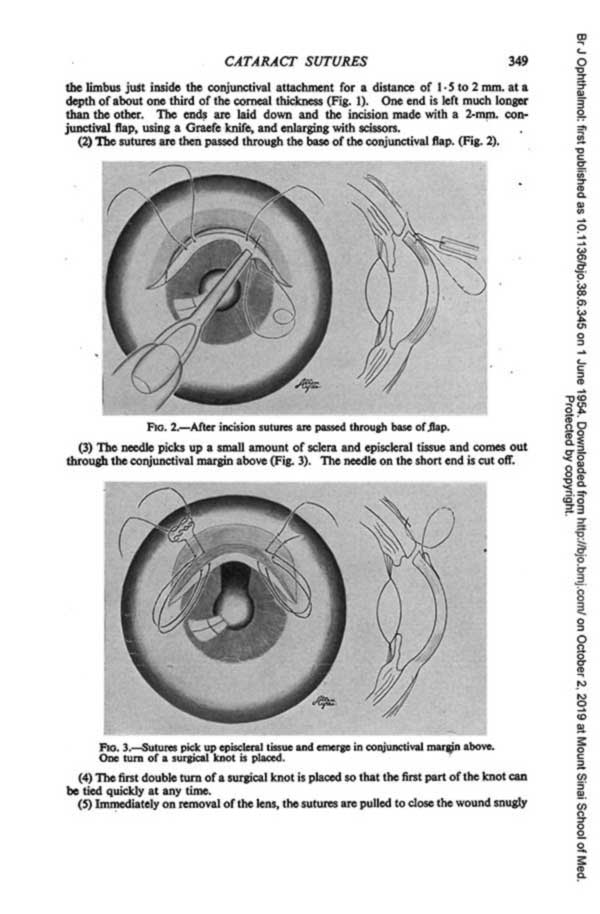
Absorbable sutures for cataract surgery are introduced by NYEE physicians Drs. Wendell Hughes, Hunter Romaine and Loren Guy.

1946
NYEE affiliates with New York University.

1947
Dr. Algernon B. Reese, NYEE resident class of 1925, contributes to the field of ocular oncology, including the recognition, classification, diagnosis, and treatment of retinoblastoma, research into retrolental fibroplasia, and classifications of ocular melanomas. In 1947 he establishes the Department of Ocular Pathology, more recently known as the Algernon Reese Pathology Laboratory, at Columbia University’s Vagelos College of Physicians and Surgeons.
1947
NYEE establishes the first Department of Hearing Testing, now the Department of Communicative Sciences, as an outgrowth of the World War II military aural rehabilitation center.

1948
The American Board of Ophthalmology ranks NYEE as one of only three A+ hospitals for residency training in the U.S.

1949
NYEE enters into a teaching affiliation with NYU/Bellevue Medical Center.

1949
NYEE-trained Dr. Louis J. Girard conducts the first clinical investigation of corneal contact lenses.

1951
NYEE obtains a charter for its School of Otolaryngology.
NYEE reactivates the Department of Research.
NYEE opens the Maxillo-Facial Plastic Clinic.

1951
Dr. Berens and U.S. Marine Corps Captain Dr. Jerry Hart Jacobson conduct pioneering clinical studies of electroretinography at NYEE.
1954
Dr. Girard is the first ophthalmologist to perform and document corneoscleral transplantation.
1957
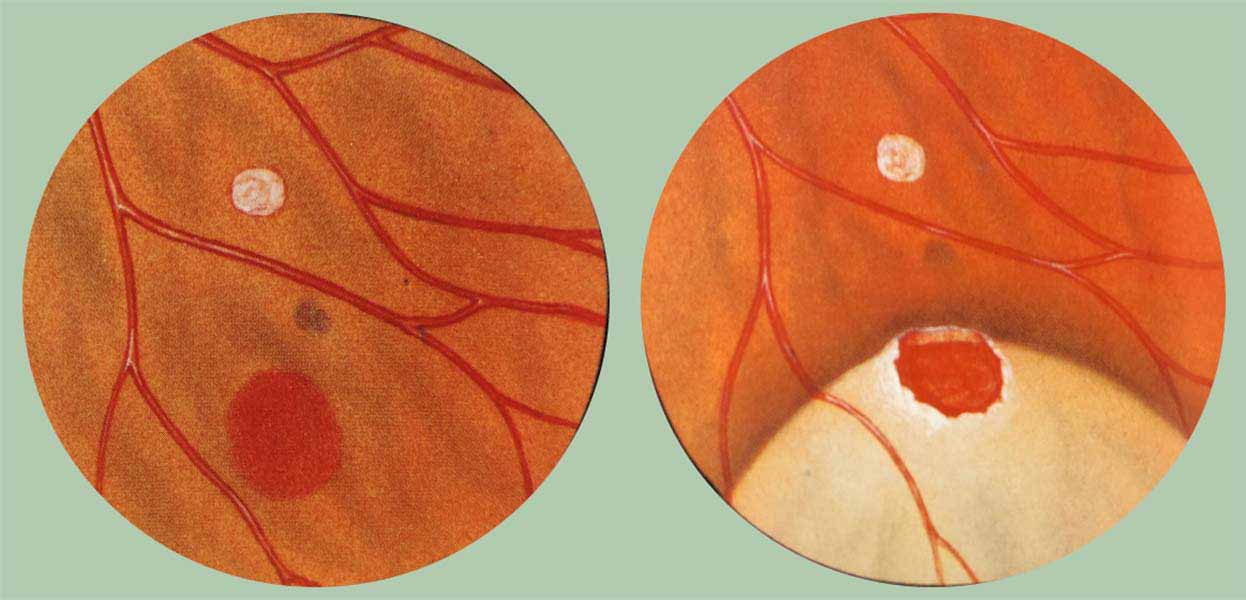
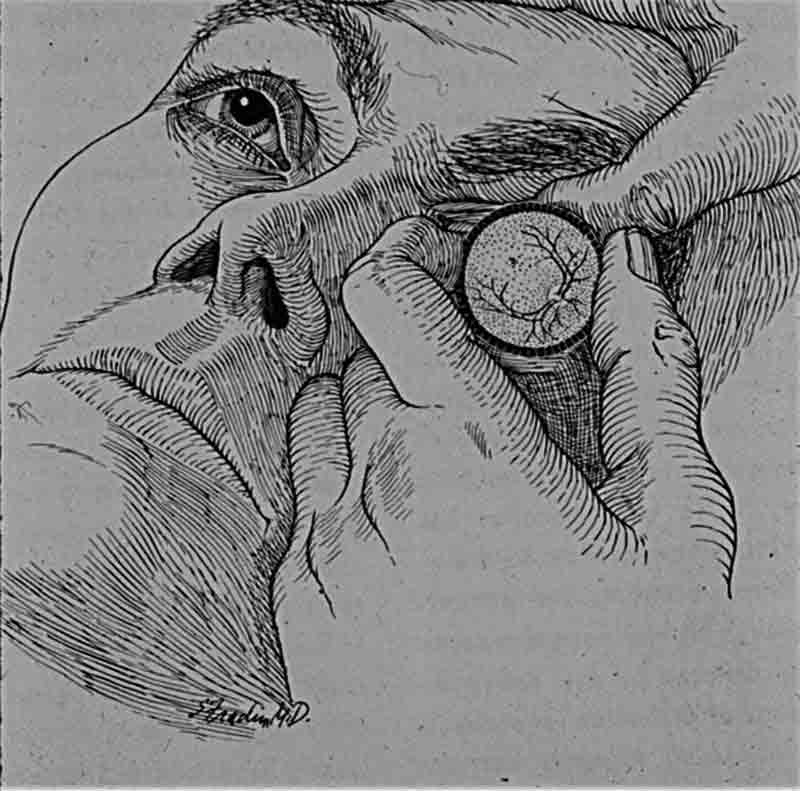
New York City’s first Retina Service is formally established at NYEE by Dr. Morton L Rosenthal, who introduces techniques of indirect ophthalmoscopy and fundus drawing for visualizing the retinal periphery, ushering in a new era in modern retinal surgery.
1957
NYEE opens its new research laboratories in the renovated brownstone at 314 East 14th Street.
1958
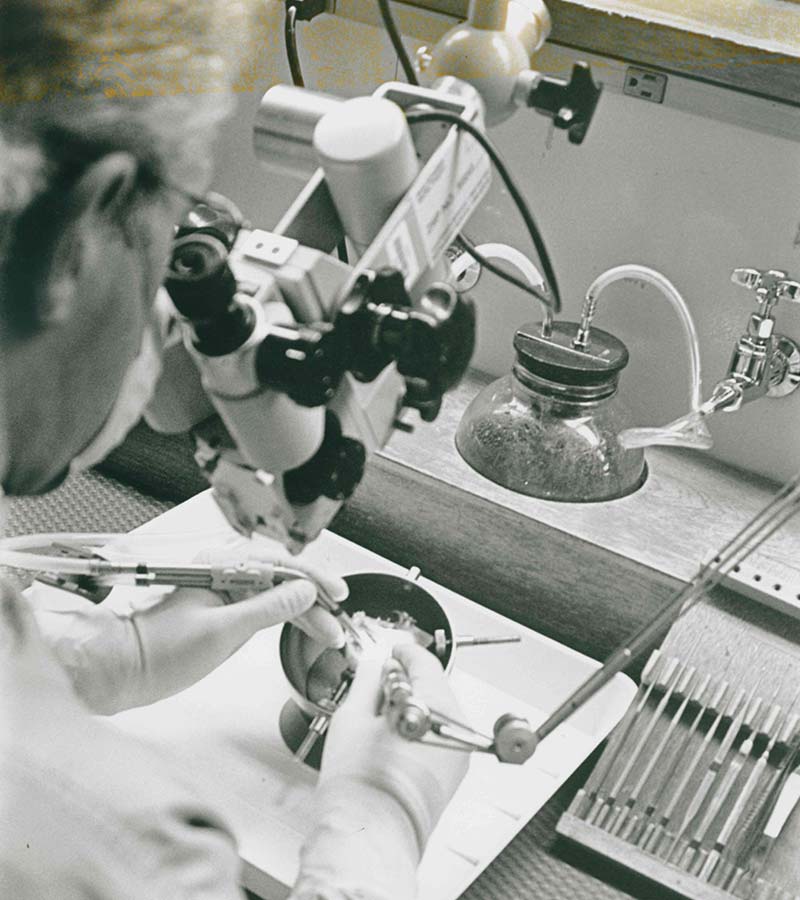
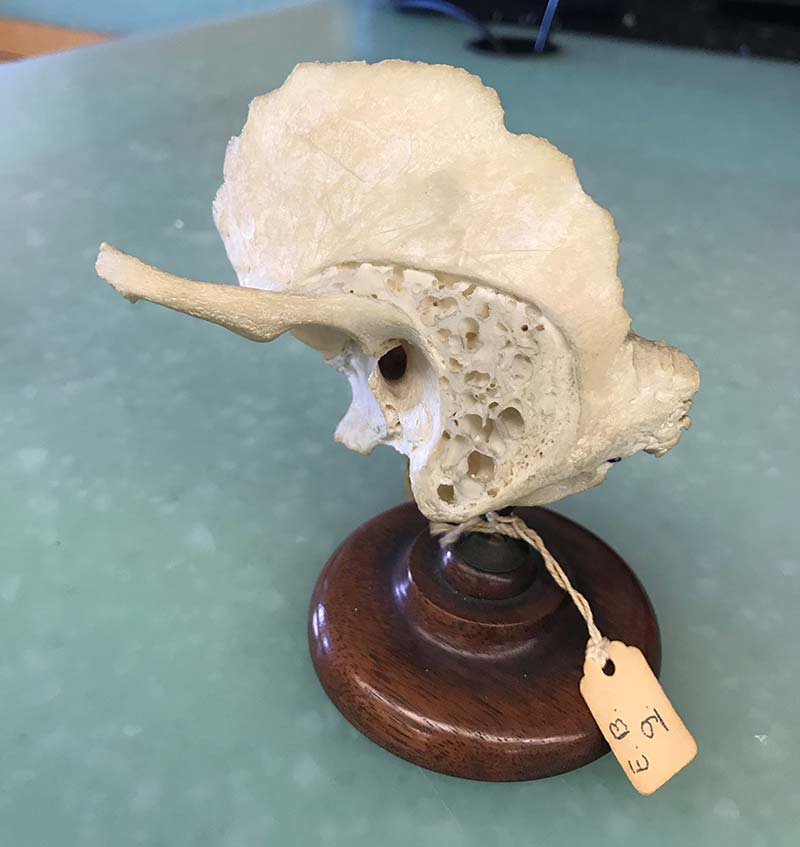
NYEE’s Temporal Bone Laboratory, the first on the East Coast, is established to train otolaryngologists in temporal bone surgery.

1958
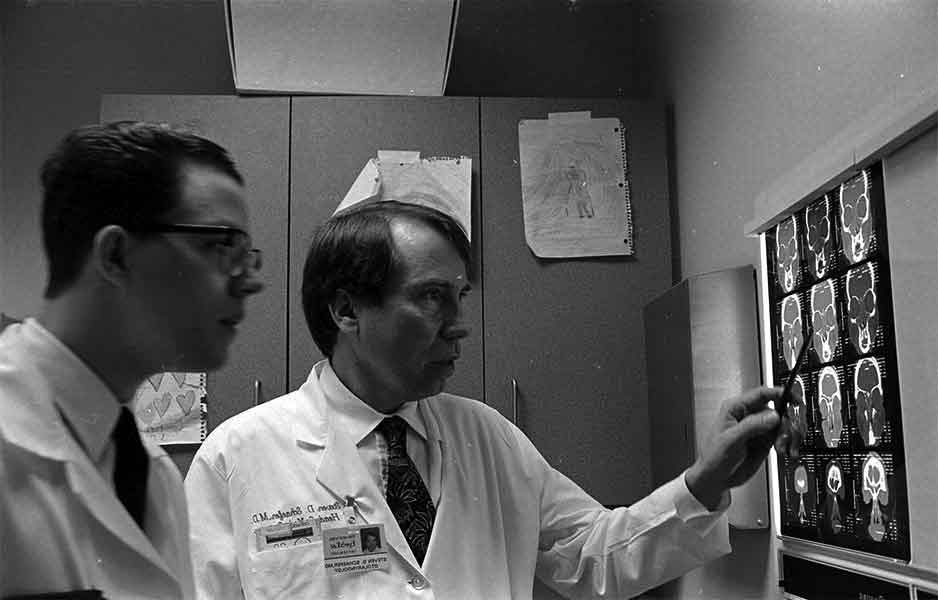
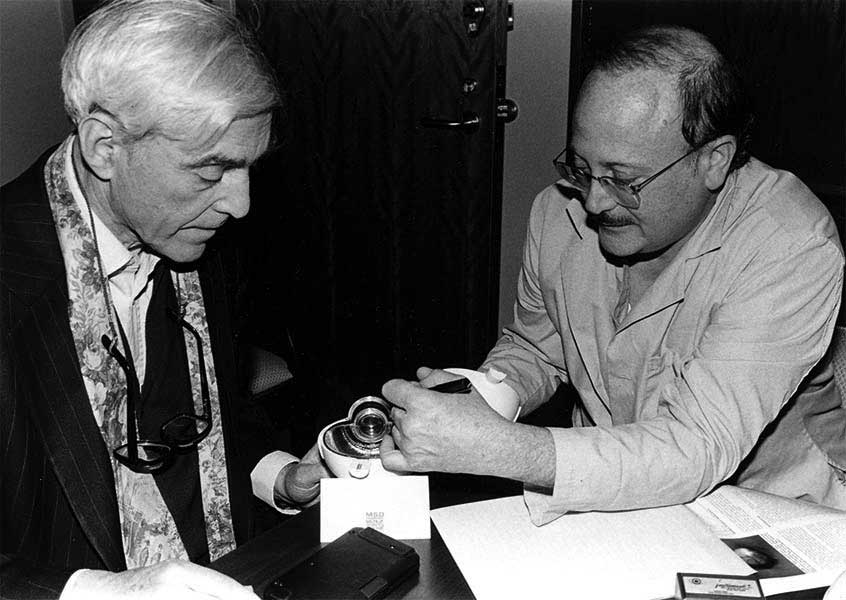
NYEE’s Center for Electroretinography is established by Drs. Jerry Jacobson and Weeks (pictured) on the 5th floor of the South Building. Dr. Jacobson became a leading contributor to the development and standardization of clinical electroretinography.

1958
NYEE’s Cornea and Glaucoma Subspecialty Services are created.

1958
Dr. Girard, co-designs the first small, thin contact lens.
1959
Dr. Bruno S. Priestley, an NYEE physician, establishes the Department of Pleoptics – the first of its kind in the U.S. and the largest of its kind in the Western Hemisphere.

1960
NYEE’s Social Service Department hires its first multilingual employee, who is fluent in English, Spanish, and Italian.

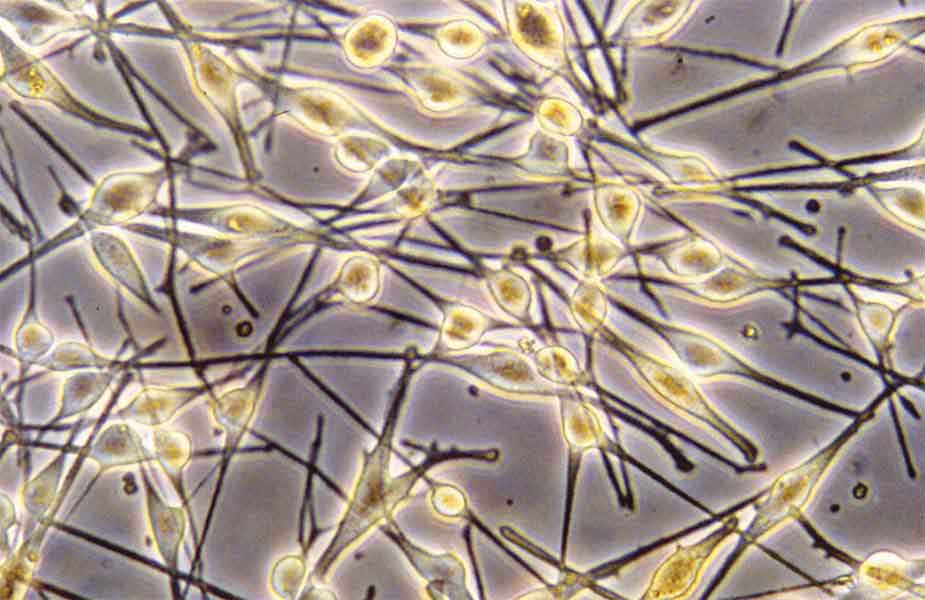
1961
Drs. Rosenthal and Seymour Fradin, along with Dr. Charles Townes and Nobel Prize winning physicist Arthur Leonard Schawlow, conduct early studies of laser photocoagulation in rabbit retinas at Bell Labs that would eventually become the mainstay treatment for diabetic retinopathy.
1964
In 1958, Dr. Aran Safir, during his NYEE residency, invents an early electronic retinoscope. Six years later, he receives a patent for his invention.
1966
“The Technique of Binocular Indirect Ophthalmoscopy,” a seminal article authored by Drs. Rosenthal and Fradin, published in Highlights of Ophthalmology with illustrations by Fradin, establishes a methodology for retinal exams still in use today.

1967
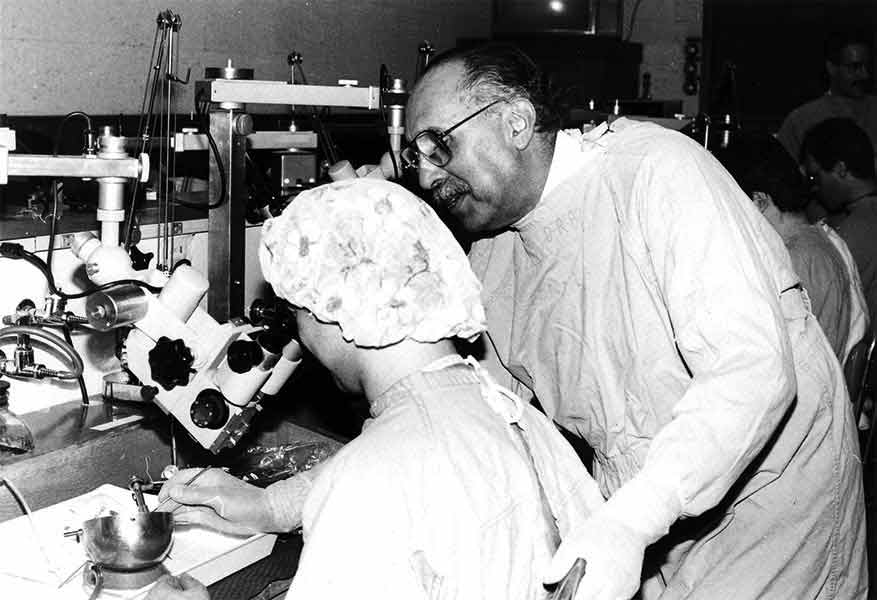
Dr. Charles D. Kelman, an NYEE physician, devises the first revolutionary apparatus for phacoemulsification used in cataract surgery.
1967
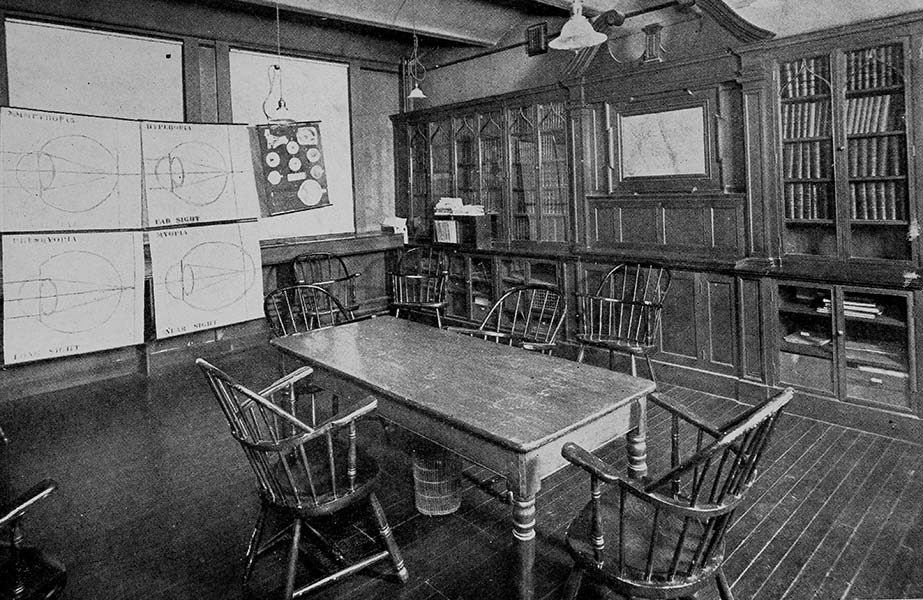
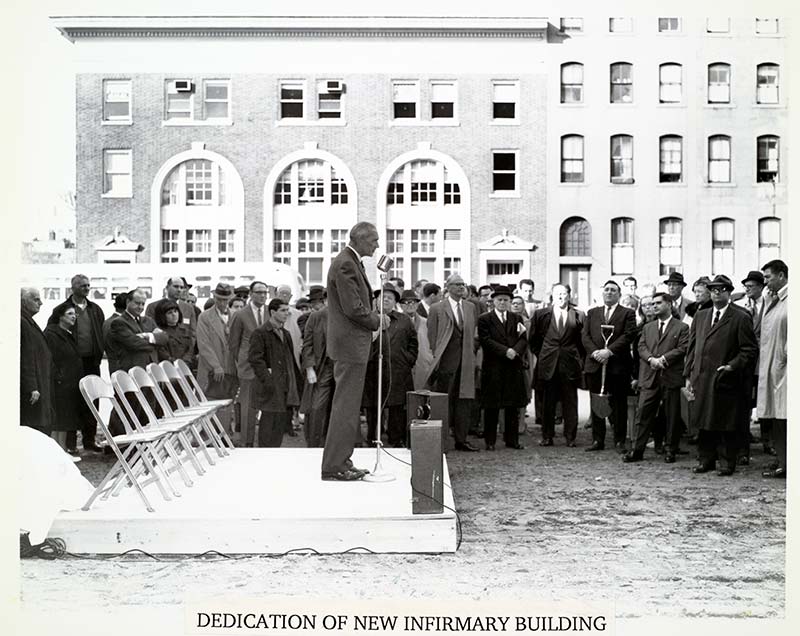
NYEE dedicates its new North Building on East 14th Street. The original South Building is renovated and modernized to house the Eye Clinic, subspecialty services, a lecture hall, and private physician offices.

1967
NYEE attending Dr. Norman B. Jaffe was among the first three surgeons in the U.S. to implant an intraocular lens following cataract extraction. Dr. Jaffe went on to become a seminal figure in the development of modern cataract surgical techniques.

1968
NYEE opens its new North Building on East 14th Street with 207 beds and 10 state-of-the-art operating suites.

1970
NYEE celebrates 150 years of service.
1971
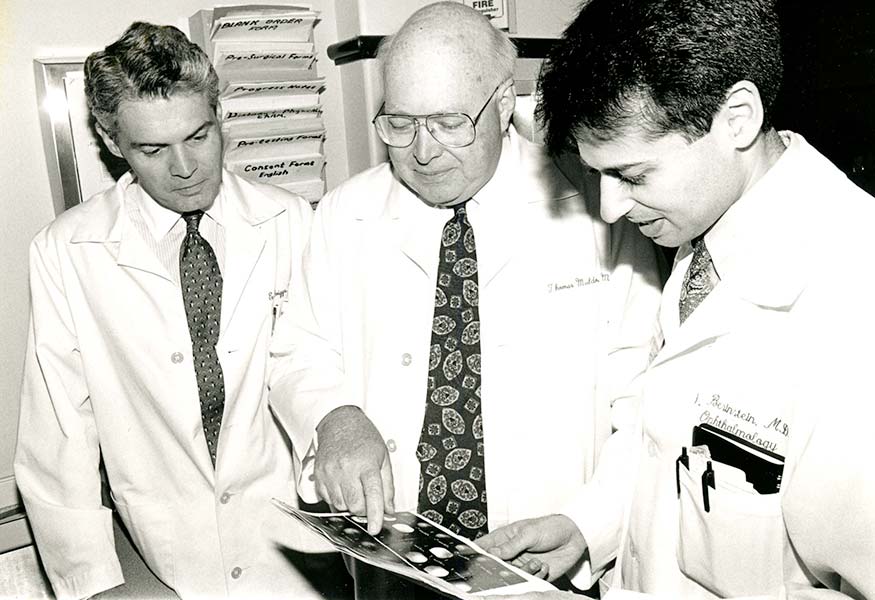
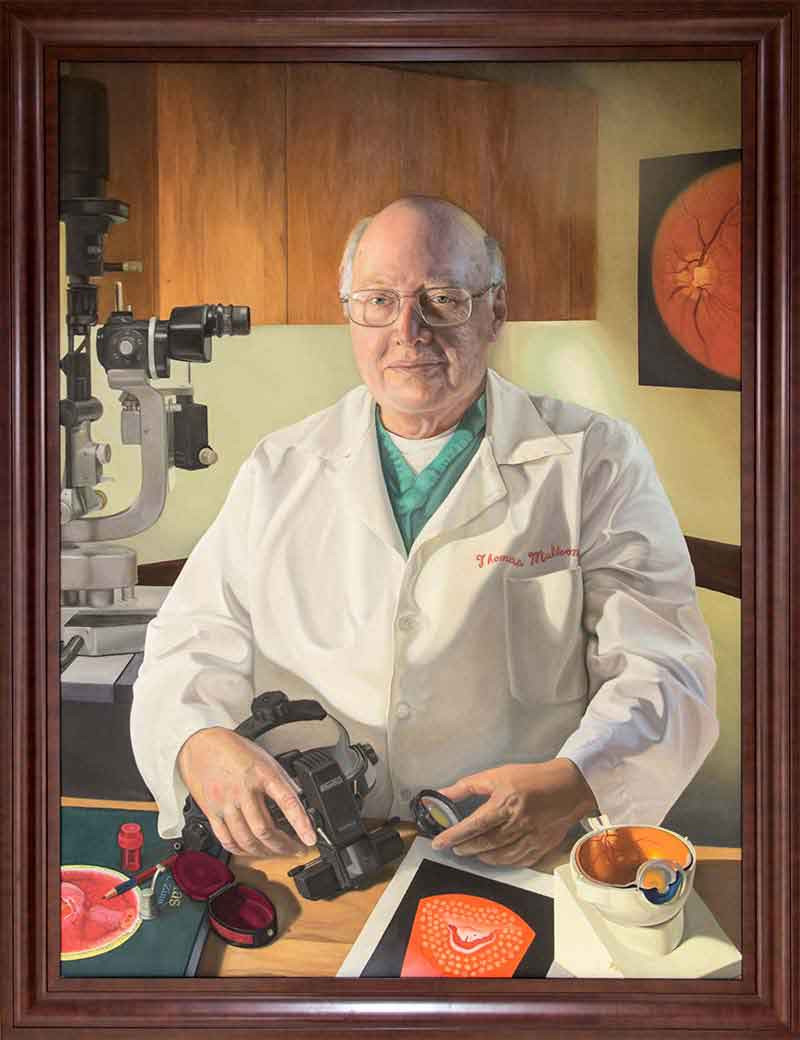
The NYEE Retina Diagnostic Center, incorporating retinal photography and fluorescein angiography, is established by Dr. Thomas O. Muldoon, NYEE resident class of 1966.
1972
Dr. Young Bin Choo, otolaryngologist and NYEE alumnus, is awarded a $85,000 Guggenheim Foundation grant to construct an 11-station, state-of-the-art Temporal Bone Laboratory. The only other laboratory of its kind anywhere in the world was located at the House Ontology Group in Los Angeles, California. Both were designed by Jack Urban.

1974
The NYEE Staff Residence Building, a $5 million 14-story 123-apartment facility, opens at 321 East 13th Street.

1974
The NYEE physicians Drs. David Krohn, Donald Morris, and Ron Jacobs pioneer the use of hematoporphyin derivatives for diagnosis and photodynamic therapy of choroidal melanoma.
1977
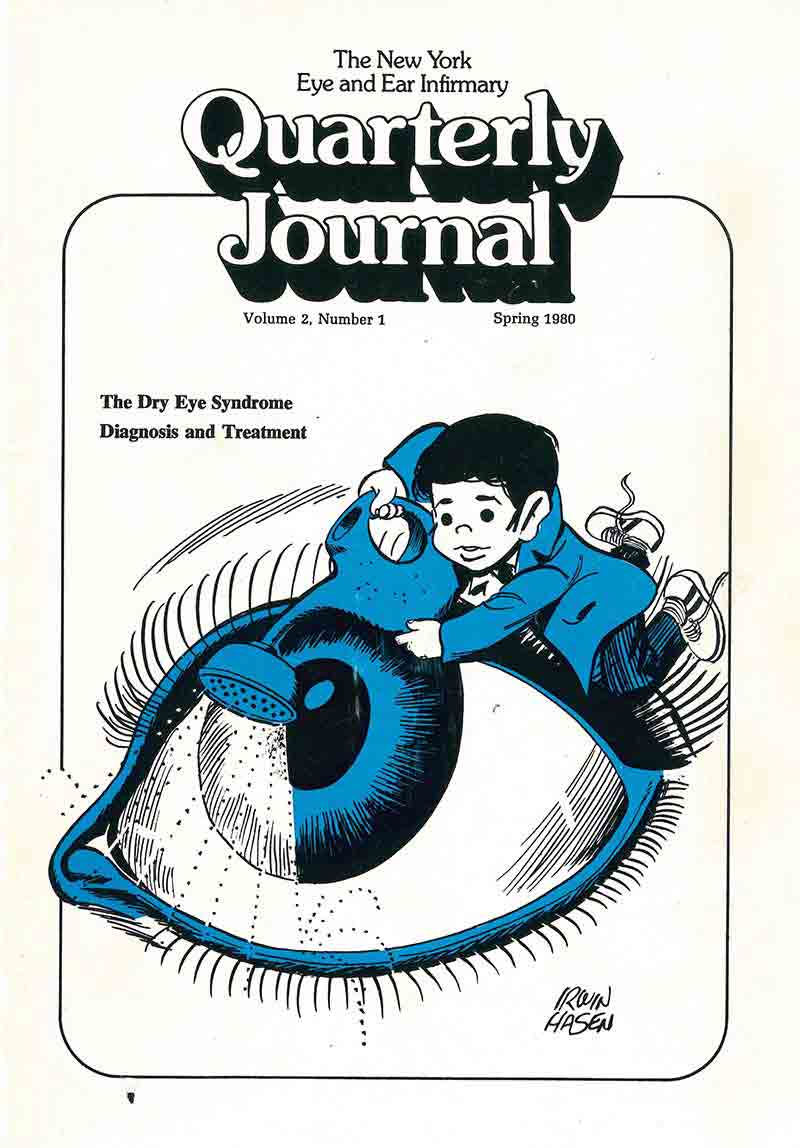
The New York Eye and Ear Infirmary Quarterly Journal is launched by Drs. Richard S. Koplin and Virginia Lubkin.
1979
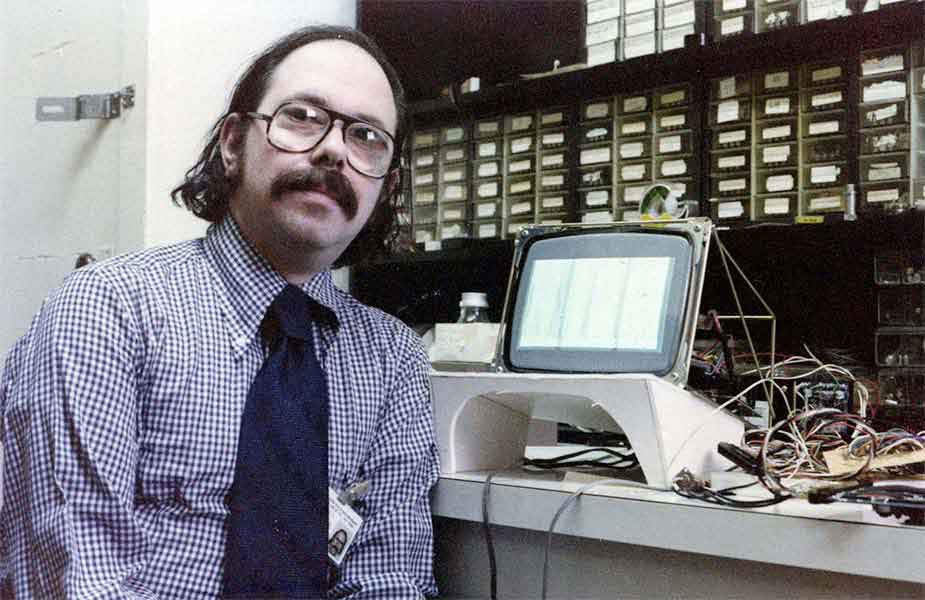
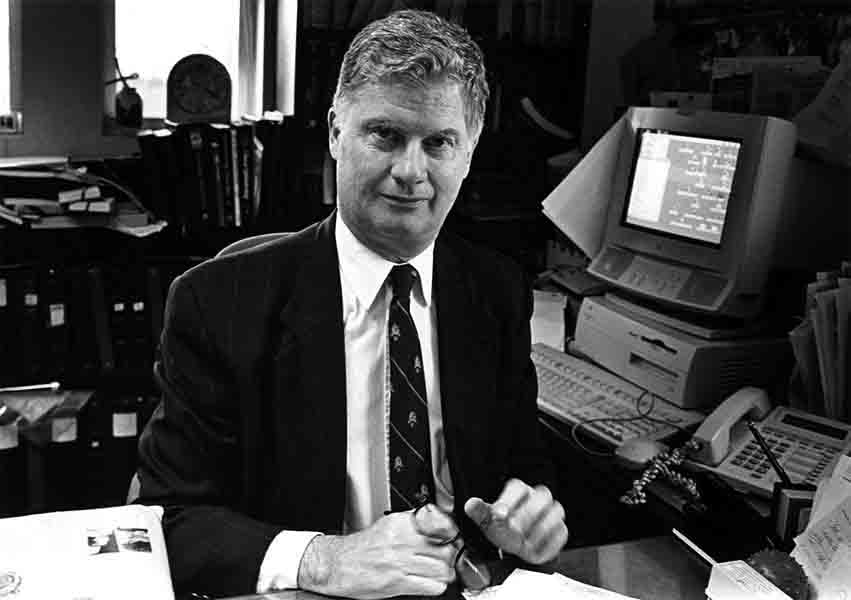
NYEE Bioengineering and Computer Science Division is established by Dr. Koplin and Martin Gersten (pictured), an engineer, and the first digital A-scan ultrasound system for intraocular lens measurements is created.
1980
NYEE affiliates with New York Medical College and Dr. Michael Dunn becomes the first chair of ophthalmology.
1982
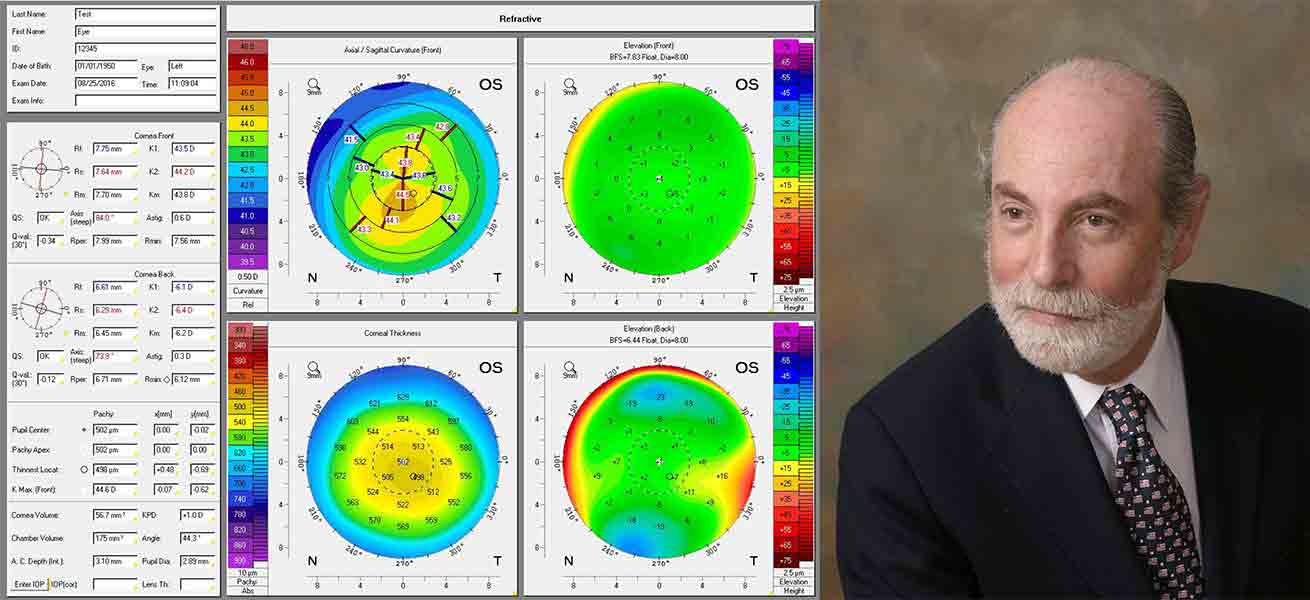
A team of clinician-scientists at NYEE, Dr. Lubkin, Martin Gersten, Dr. Koplin (pictured), and Dennis Gormley, invented corneal topography and built the first corneal mapper, leading the way to precision corneal vision correction.

1983
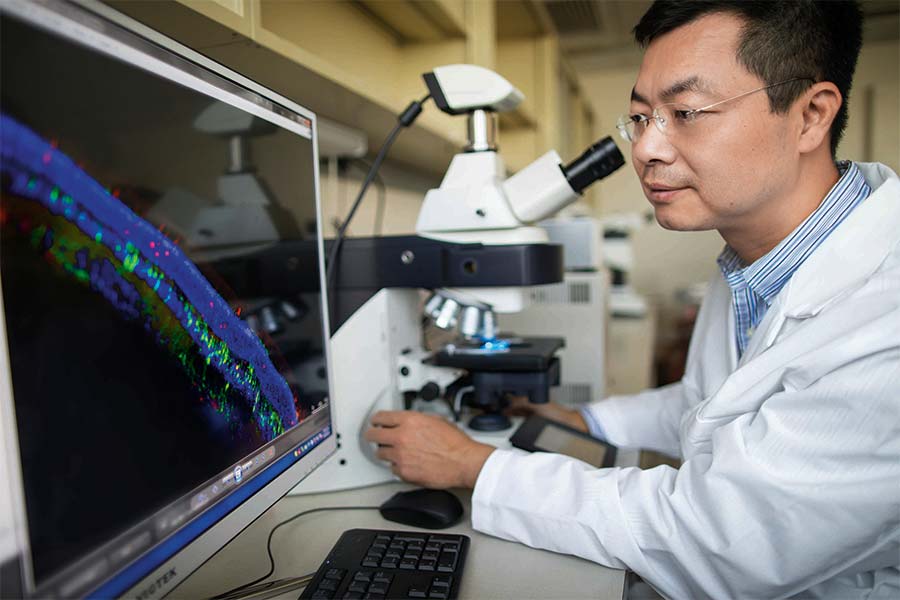
Dr. Robert Ritch joins the NYEE staff, expanding glaucoma research and creating the Ocular Imaging Center for the study of optic nerve structure and blood flow. The Center becomes a world-class glaucoma imaging-resource with the advent of high-resolution ultrasound biomicroscopy (1994) for investigating the anterior segment anomalies such as plateau iris, and (1995) employs one of the first OCT systems outside MIT, where it was developed.

1983
NYEE’s Department of Plastic and Reconstructive Surgery is created by Dr. Donald Wood-Smith.
1984
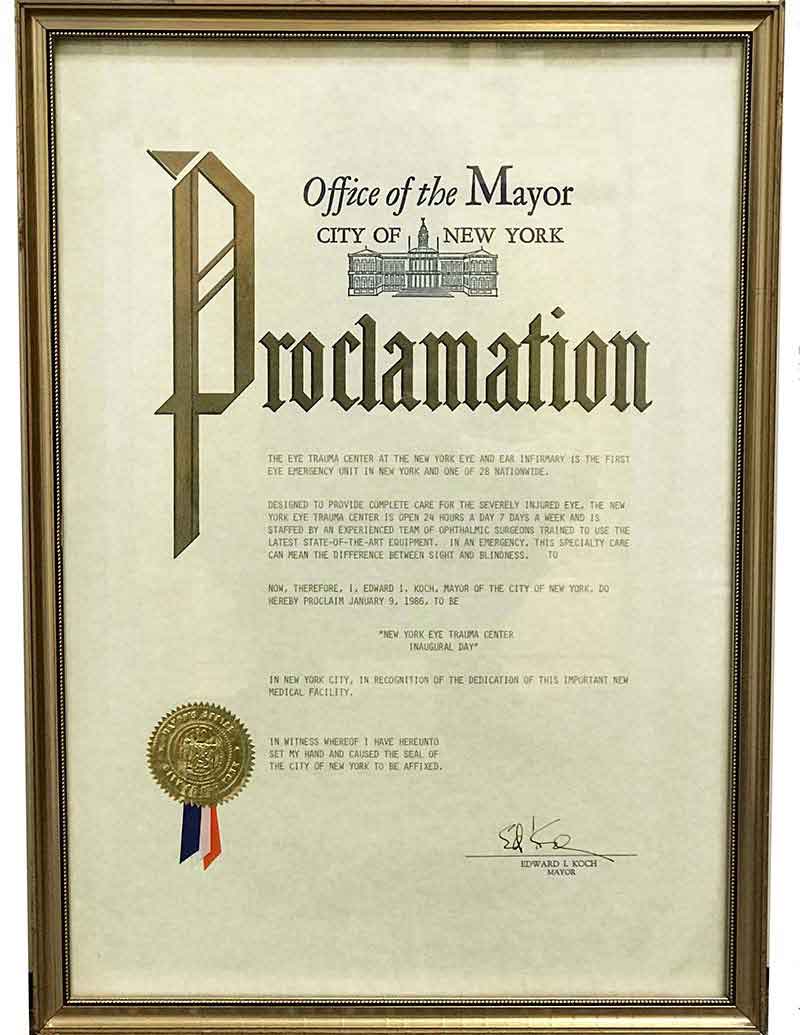
The New York Eye Trauma Center, the first of its kind in New York City, opens at NYEE under the leadership of Dr. Koplin.

1985
NYEE establishes New York City’s first inpatient Diabetes Treatment Center, offering integrative care for patients with diabetes vision-related problems.
1987
Drs. Safir and Leonard Flom patent their idea for an iris identification system, basing it on the idea that no two irises are alike.

1988
NYEE’s Bioengineering and Computer Science Division becomes the Aborn Laboratory.

1988
The first commercial manufactured corneal mapping device TMS-1, invented in NYEE’s Bioengineering and Computer Science Laboratory, is introduced. It leads the way to precision corneal vision correction and is still widely in use today.
1988
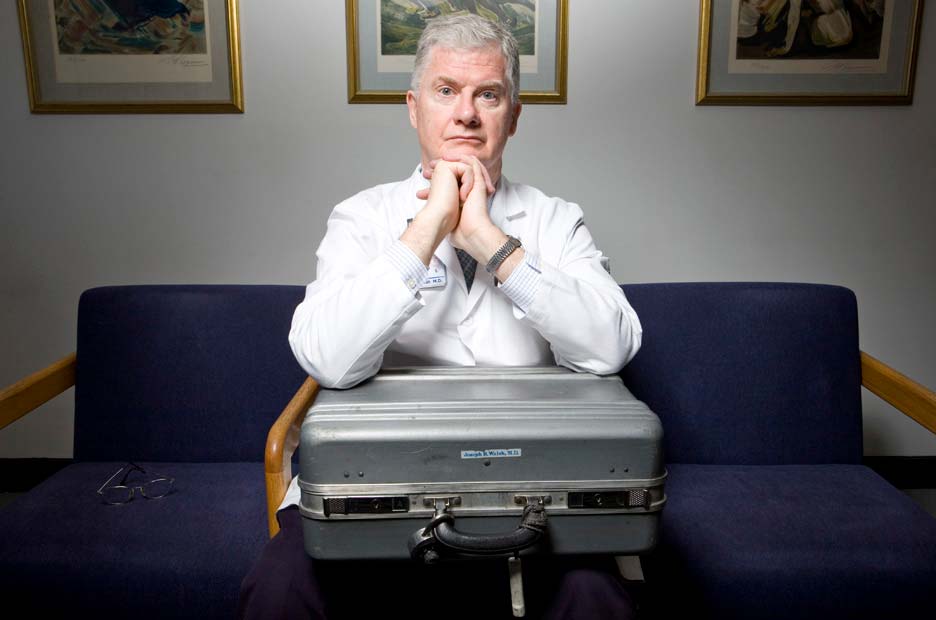
Dr. Joseph B. Walsh becomes NYEE’s second Chairman of Ophthalmology.
1989
Endoscopic sinus surgery is pioneered by NYEE otolaryngology chair Dr. Steven D. Schaefer.
1990
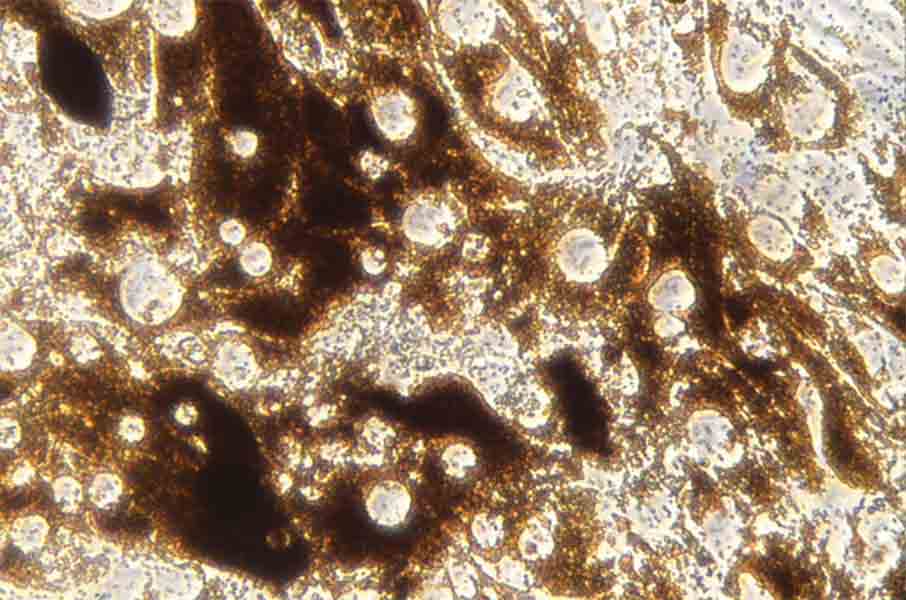
Drs. Dan Ning Hu, Ritch, and Steven A. McCormick, Chief of Pathology, develop the first successful methodology for isolation and culture of human iris pigment epithelial cells at NYEE’s Ocular Cell Cultural Laboratory.
1990
NYEE is the first to use apraclonidine, an anti-glaucoma drug, in the U.S.
Department of Communicative Disorders at NYEE offers speech therapy in Spanish to better serve Hispanic patients in the Infirmary’s service area.

1991
NYEE create an inpatient Diabetes Treatment Center program for intensive patient rehabilitation and education.
NYEE’s Outpatient EYE and ENT Centers open following a major update and redesign.
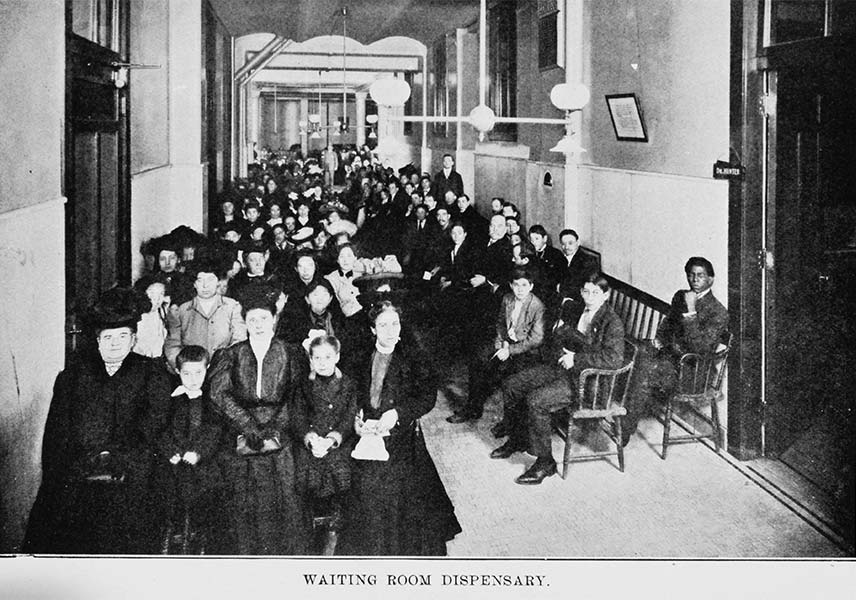
With 70,000 eye visits annually, NYEE comprises the largest clinic volume in the U.S. and the largest provider of primary eye care in the New York Metropolitan area.
With 51,902 ENT patients, the NYEE’s Department of Otolaryngology/Head & Neck Surgery is the largest collection point of clinical material of any facility in North America.
1992
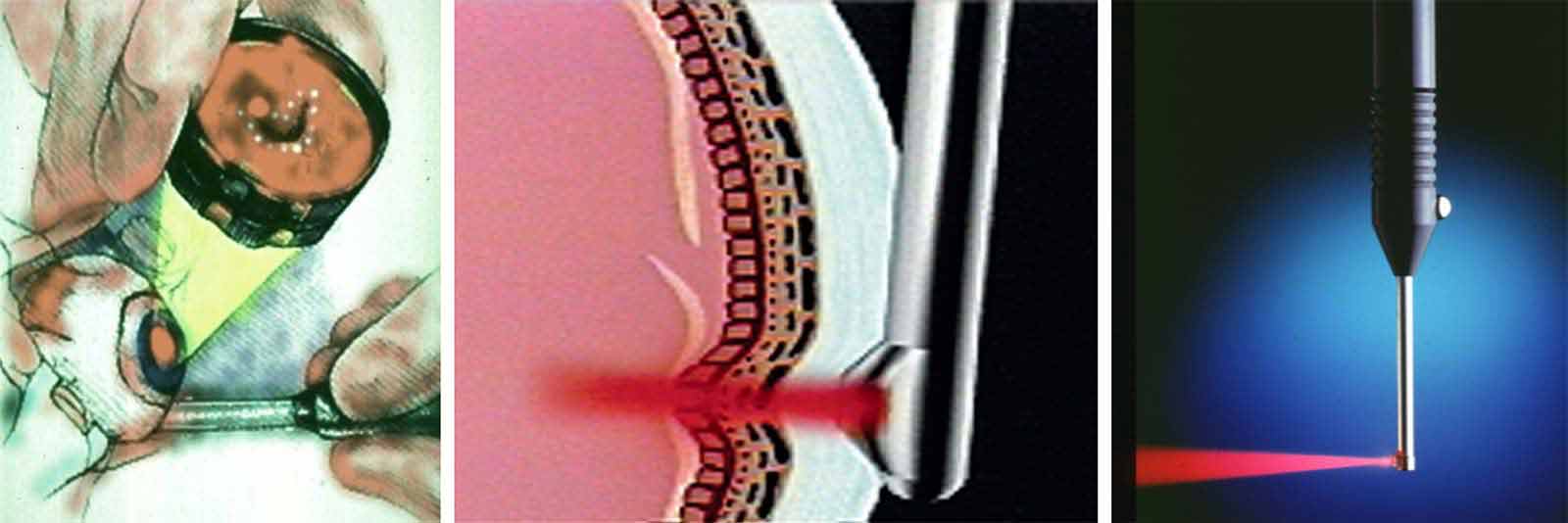
Drs. Rosen and Muldoon, and David Buzawa, an engineer, along with a team from Iris Medical, develop the first commercial trans-scleral laser retinopexy probe for repairing retinal tears and detachments.

1992
NYEE opens New York City’s first pediatric glaucoma clinic.
1992
Drs. Hu, Ritch, and Steven A. McCormick create NYEE’s Ocular Cell Culture Lab and develop the methodology for isolation and culture of human uveal melanocytes. Exfoliation material is identified in tissue culture for the first time in cells extracted from glaucoma patients diagnosed with exfoliation syndrome.

1992
The New York Eye and Ear Infirmary Ophthalmology Associates, P.C., a self-sustaining organization for resident education and patient care, is formed to leverage the expertise of the Infirmary’s large voluntary teaching staff of community ophthalmologists.

1992
NYEE’s Ambulatory Surgery Center is created, utilizing a full floor for pre-and post-operative patient management adjacent to operating and recovery rooms, enabling throughput of more than 100 surgical cases per day.

1992
NYEE neuro-otologist Dr. Christopher L. Linstrom performs the Infirmary’s first cochlear implant on 10-year old Alex Carrasco.
1992
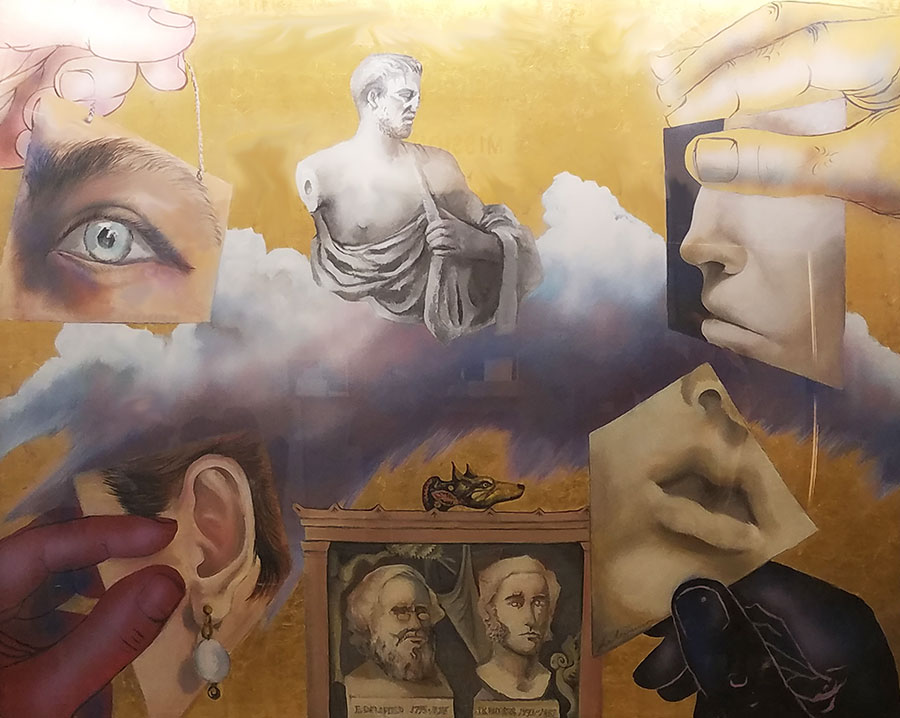
NYEE acquires “Homage to Hippocrates,” a mural-sized painting by artist Harold Stevenson, donated by Board Member Anastasios Karavias.

1995
NYEE celebrates its 175th anniversary.
1995
Dr. Ritch demonstrates that laser therapy is a safe and effective alternative to eye drops as a first-line treatment for patients with newly diagnosed primary open-angle glaucoma.

1995
NYEE establishes New York City’s first hospital-based hearing aid dispensary.
NYEE receives New York City’s first OCT imaging device.

1996
3-D ultrasound biomicroscopy (UBM) imaging is developed by Drs. Ray Iezzi, Rosen, Celso Tello, and Ritch for volumetric visualization of anterior segment eye trauma and tumors.
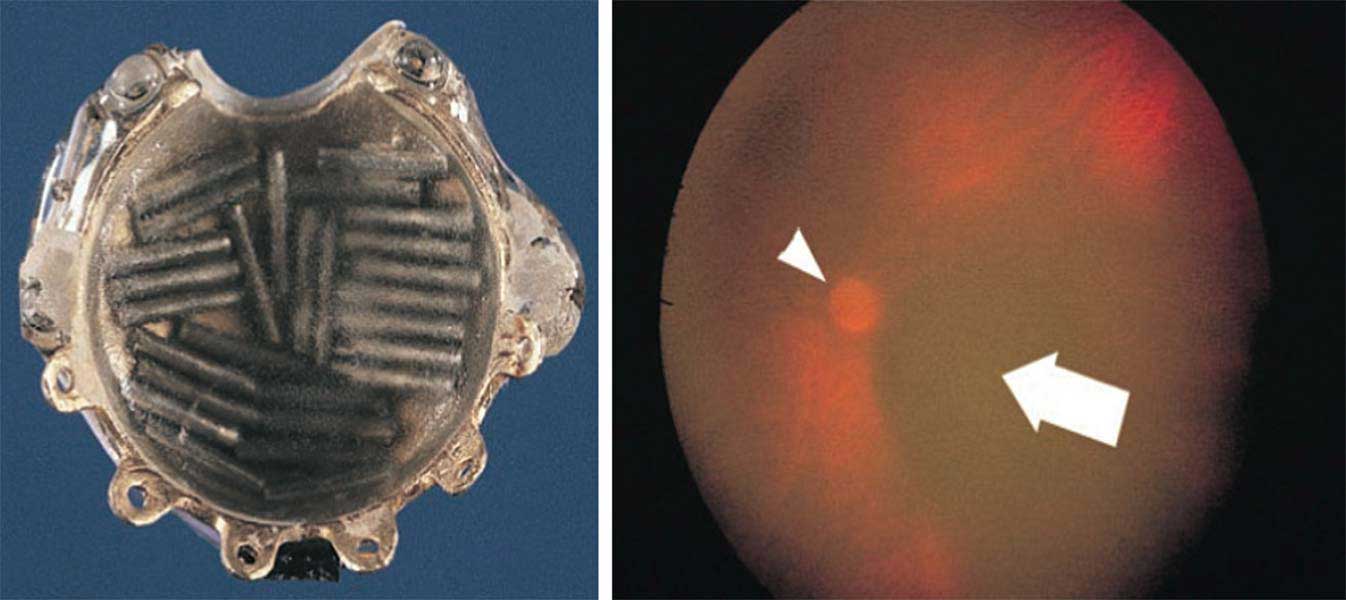
1996
Drs. Paul T. Finger, Iezzi, Rosen, and Eliot L. Berson introduce self-illuminating branchytherapy plaques, enabling improved precision in the placement of radioactive plaques implanted for treatment of sub-macular choroidal melanomas.
1997
Dr. Muldoon, an early champion of advanced retinal diagnostics and therapeutics such as fluorescein angiography, ultrasound, laser, and vitrectomy, becomes the second Chief of NYEE’s Retina Service.

1999
NYEE becomes a member of Continuum Health Partners, Inc., associating with Beth Israel Medical Center, St. Luke's Hospital, Roosevelt Hospital, and Long Island College Hospital.

2002
NYEE’s Vestibular Rehabilitation Center is opened.

2002
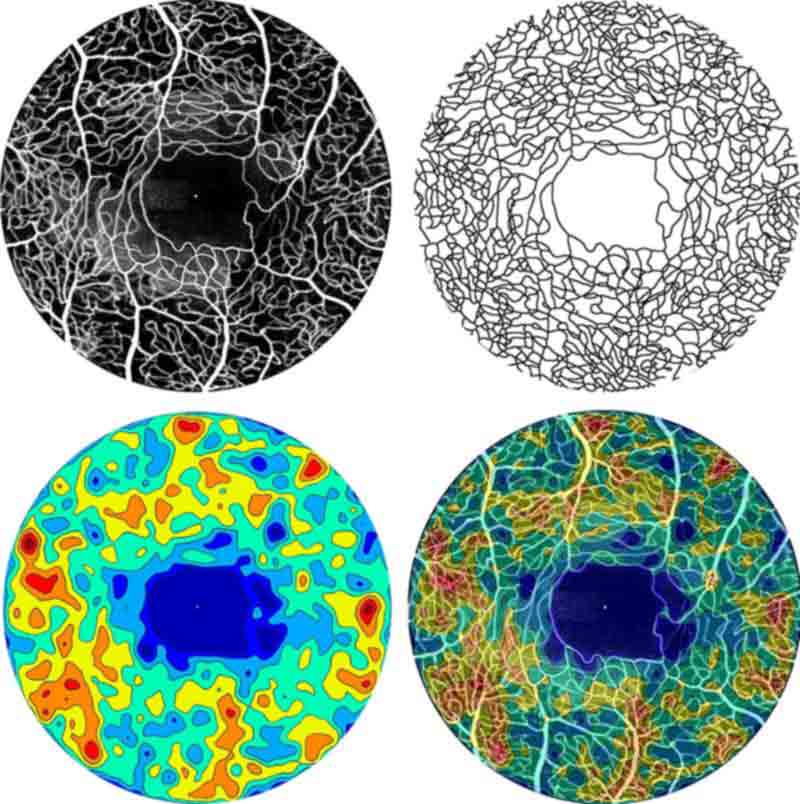
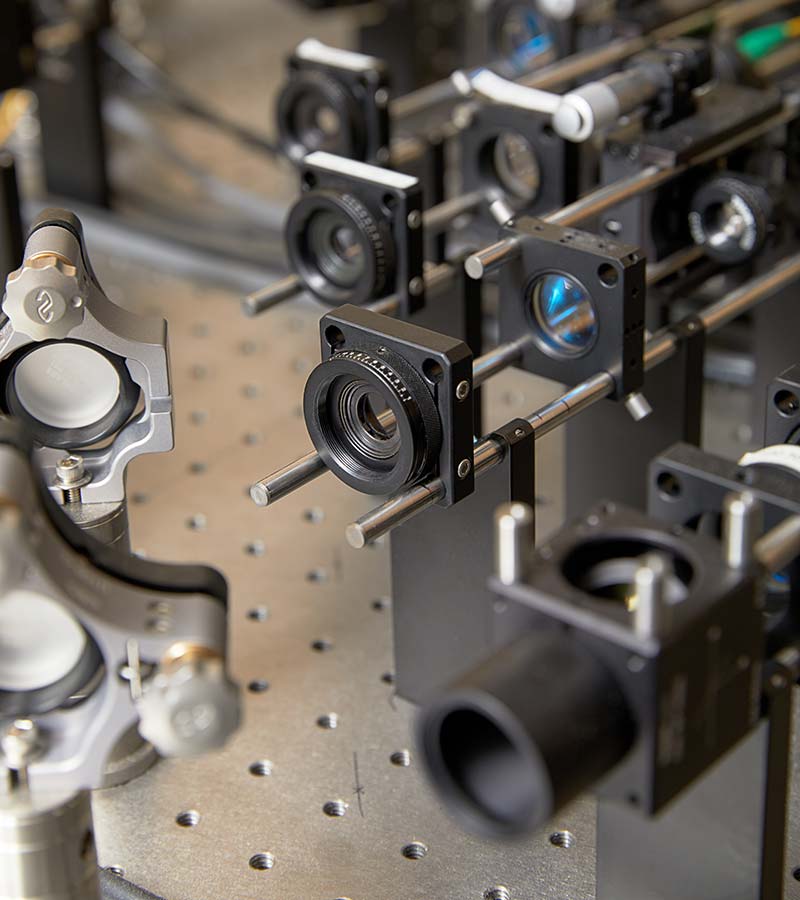
Drs. Rosen and Patricia Garcia and Mark Hathaway, and engineer Rishard Weitz, working with Drs. Adrian Podoleanu and George Dobre, combine en face OCT/Confocal Scanning Laser Ophthalmoscope (SLO), developed at the University of Kent, with idocyanine green angiography (ICG) to create simultaneous multi-channel OCT/SLO/ICG angiography.

2003
NYEE opens the Bendheim Family Retina Center, a 10,000 square foot floor dedicated to state-of-the-art diagnosis and treatment of retinal disease.

2003
NYEE Aborn Laboratory is renamed the Aborn-Lubkin Laboratory in memory of Dr. Lubkin, its founder.

2004
NYEE opens the Jorge N. Buxton, MD, Microsurgical Education Center.

2005
NYEE’s Sleep Center is created.

2005
NYEE holds the “Eye on the Future” colloquium, the first of its kind to bring together specialists focusing on the future of organ, tissue and eye transplantation and donation.

2005
Drs. Joseph Arigo and George Alexiades (pictured) successfully perform the tri-state area’s first fully implantable hearing aid surgery.

2006
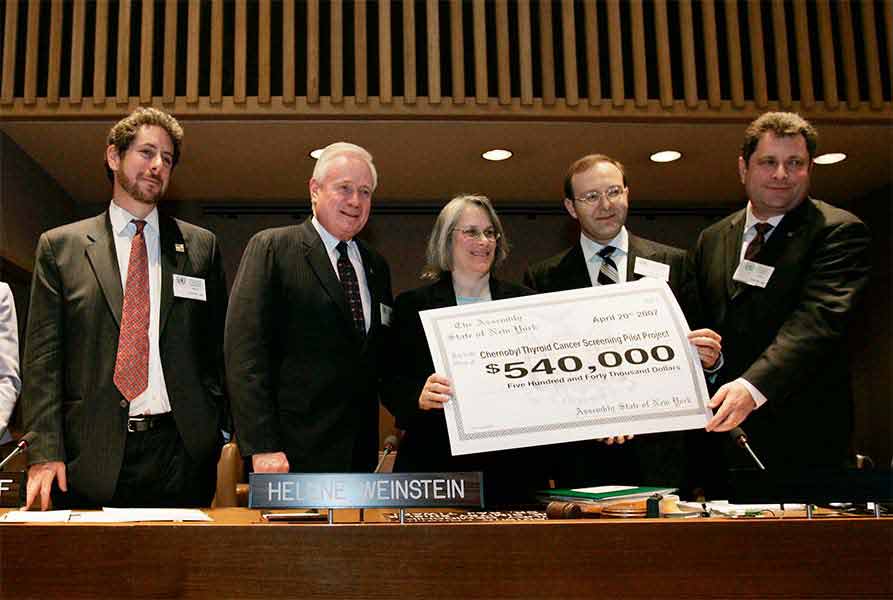
The Otolaryngology Department at NYEE organizes an international conference at the United Nations to address radiation-induced thyroid cancer related to the Chernobyl nuclear accident.

2006
Dr. Ritch is honored as the first recipient of the Shelley and Steven Einhorn Distinguished Chair of Ophthalmology.

2006
NYEE ocular oncologist Dr. David Abramson introduces intraarterial chemotherapy in the U.S. for treatment of retinoblastoma, leading to a major shift in the management of this condition.
2007
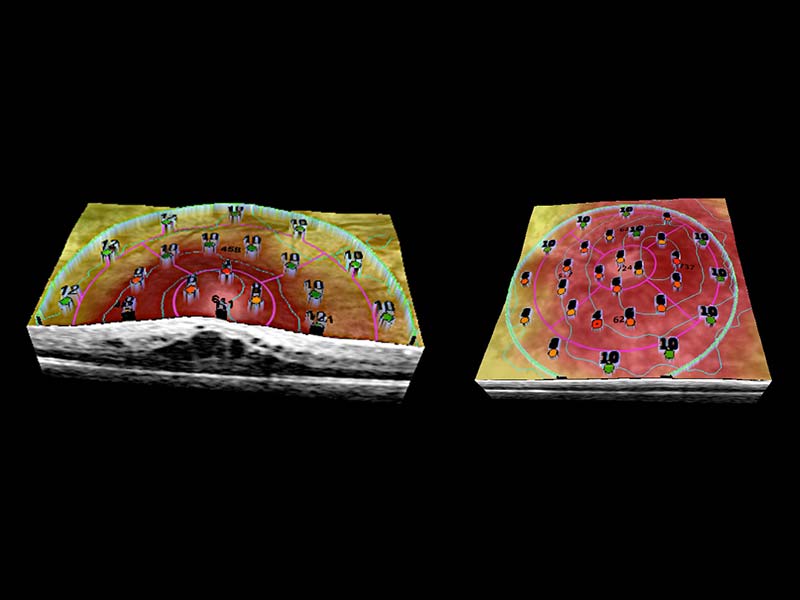
Drs. Rosen, Garcia, Gennady Landa, and Weitz, with a Toronto-based Ophthalmic Technologies Inc. team, collaborate to integrate SLO microperimetry and OCT/SLO 3-D topographic imaging, creating the first en face OCT that combines visual functional testing with 3-D structural imaging in one instrument.

2008
The Ear Institute at NYEE opens at 380 Second Avenue, centralizing the ear specialty services of New York Eye and Ear Infirmary, Beth Israel Medical Center, and the Children’s Hearing Institute.

2008
Drs. Robert Allen, Joshua Levine (pictured), and David Greenspun pioneer autologous microsurgical breast reconstruction as an alternative to traditional post-mastectomy prosthetics.

2008
Dr. Rosen, Director of Retina Service and Ophthalmic Research at NYEE, in collaboration with Dr. Mark Kupersmith, Director of Neuro-Ophthalmology and Continuum’s Department of Neurosurgery, develops the “Eye Attack Protocol” for treatment of central retinal artery occlusion.

2009
NYEE’s Facial Paralysis Rehabilitation Center opens under the directorship of Dr. Anthony Sclafani.
2009
Dr. Walsh is honored as the first Belinda Bingham Pierce and Gerald G. Pierce, MD, Distinguished Chair of Ophthalmology.

2009
Dr. Finger champions the use of vascular endothelial growth factor inhibitors for the treatment of radiation-related maculopathy and optic neuropathy following brachytherapy for eye cancers.
2009
NYEE establishes Project Chernobyl and the Thyroid Disease Center.

2010
NYEE opens the Shelley and Steven Einhorn Clinical Research Center.

2010
Dr. Ritch pioneers the use of acupuncture for “lazy eye,” anisometropic amblyopia, replacing eye patches for many older children with this vision problem.

2012
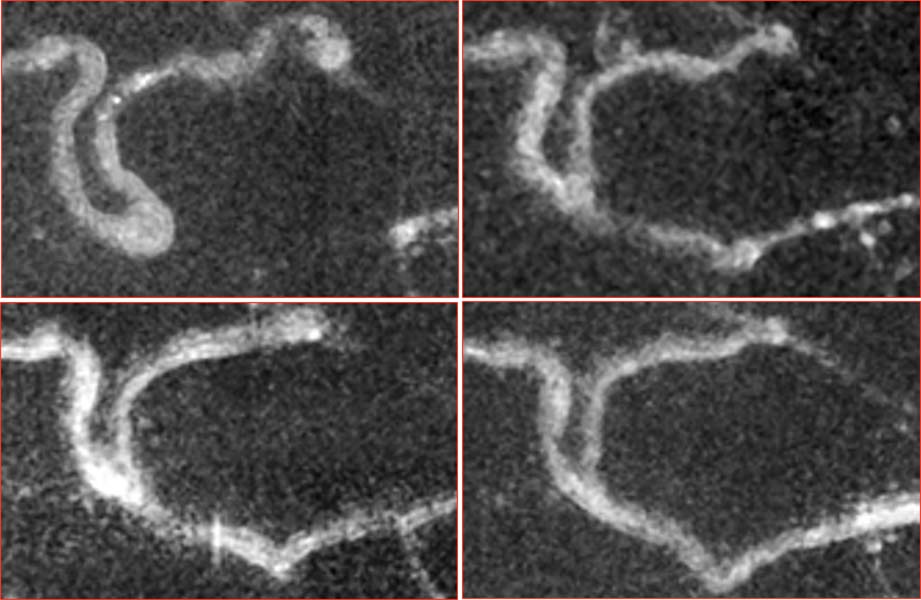
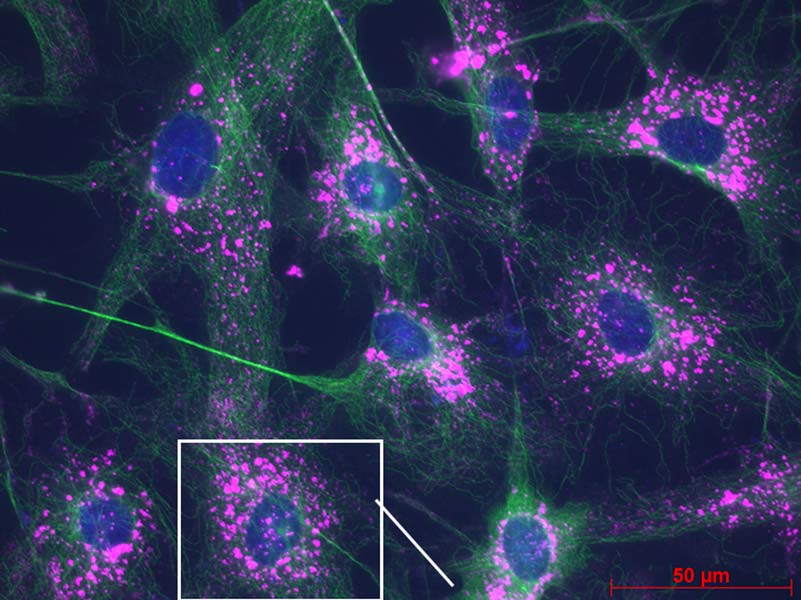
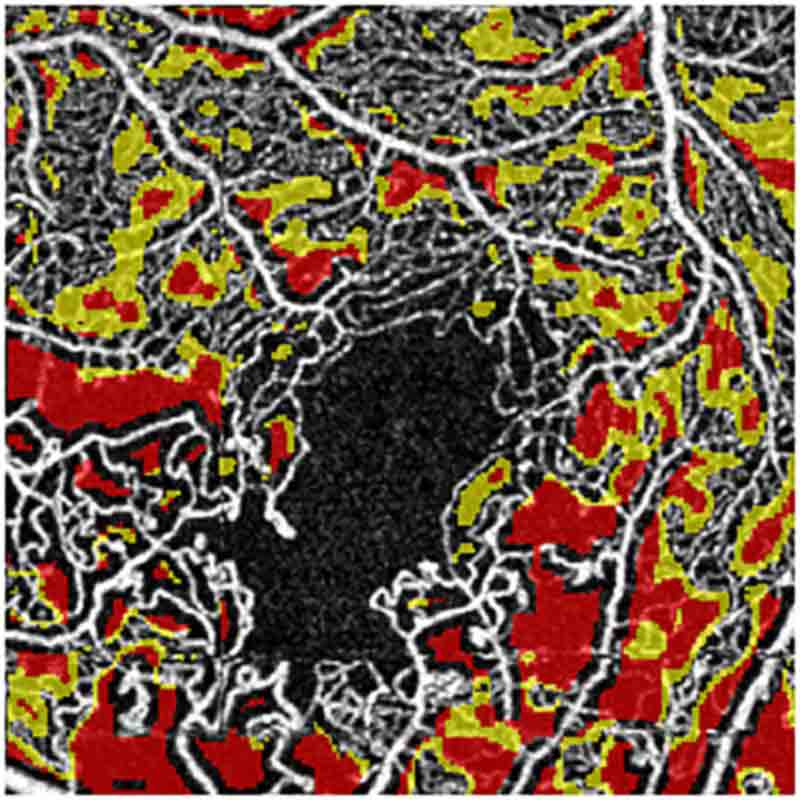
Drs. Rosen and Yuen Ping Toco Chui, under the auspices of NYEE’s David E. Marrus Adaptive Optics Laboratory and in collaboration with Drs. Alfredo Dubra and Joseph Carroll from the Medical College of Wisconsin, introduce fluorescein angiography into human adaptive optics scanning light ophthalmoscopy to further highlight changes in retinal vasculature and study the variety and the internal fluid dynamics of retinal capillary microaneurysms.

2012
NYEE expands its Post-Anesthesia Care Unit (PACU) facility adjacent to the operating suite for enhanced peri-operative care.

2013
NYEE, as member of Continuum Health Partners, Inc., merges with The Mount Sinai Medical Center, creating Mount Sinai Health System, one of the nation’s largest not-for-profit health systems and the largest nongovernment employer in New York.

2013
Ronald Gentile, MD, class of 1995, developed the cystoid dehydration of macular holes concept, which resulted in a new approach to treating macular holes using eye drops. Treatment consisted of three drops: a steroid, a non-steroidal and a carbonic anhydrate inhibitor.
2014
Dynamic histopathology, introduced by NYEE Drs. Rosen and Chui, under the auspices of NYEE’s David E. Marrus Adaptive Optics Laboratory, uses serial adaptive optics scanning light ophthalmoscopy imaging. It allows physicians to study retinal capillary microvascular remodeling longitudinally in patients at extended time intervals.
2014
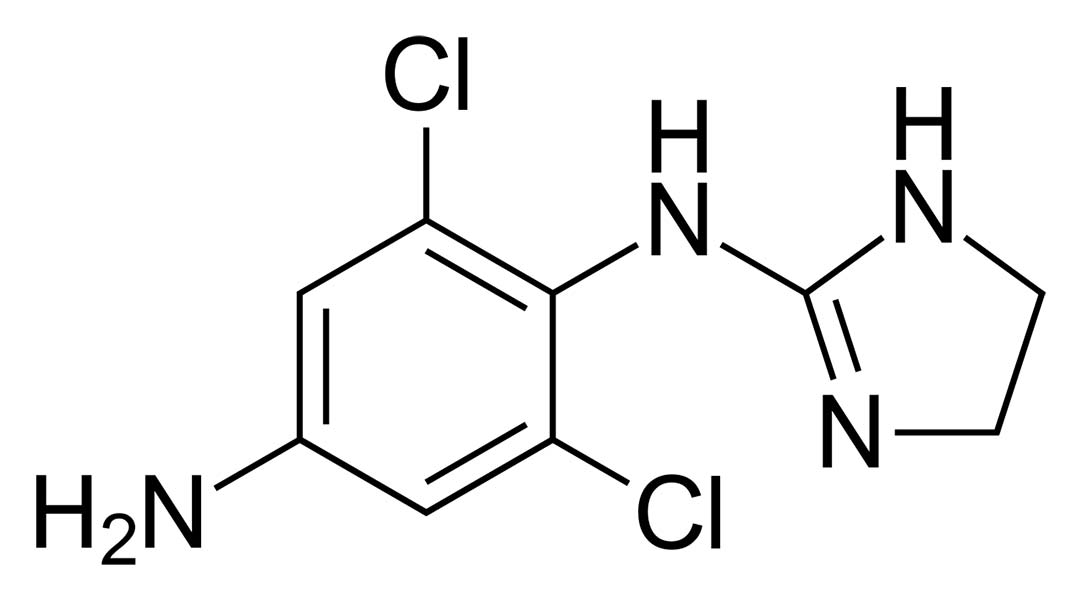
Dr. Kupersmith leads a NIH-funded study, the results of which indicate that an inexpensive glaucoma drug can preserve and actually restore vision when added to a weight-loss plan for women who develop a blinding disorder linked to obesity.

2014
Dr. Michael J. Pitman, an NYEE physician, performs the first American series of autologous temporalis fascia transplants to the vocal fold to restore patients’ voices.
2015
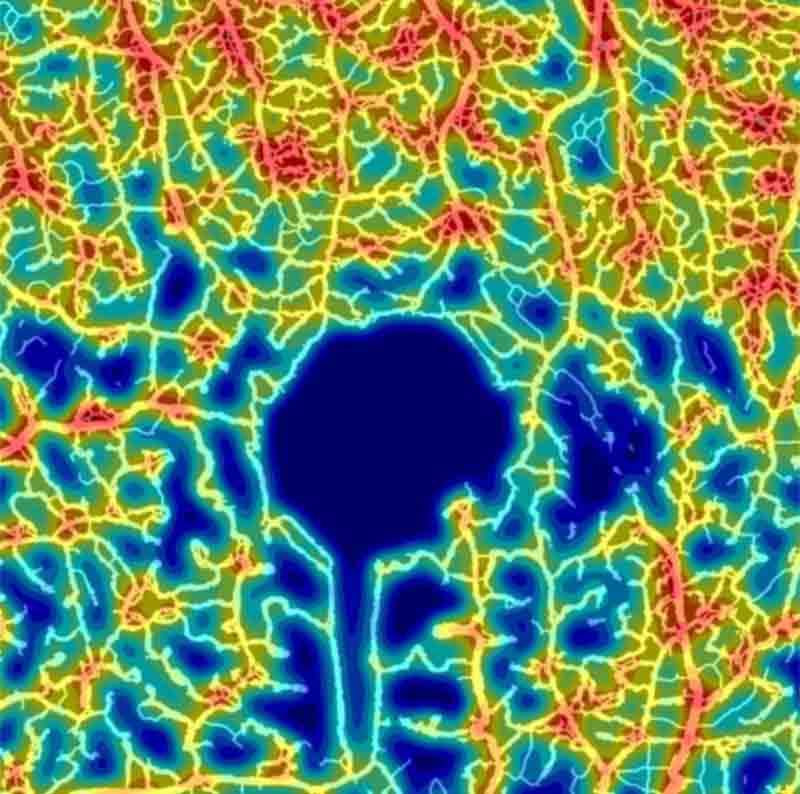
Drs. Rosen and Chui, under the auspices of NYEE’s David E. Marrus Adaptive Optics Laboratory, introduce quantitative analysis of capillary density using adaptive optics scanning light ophthalmoscopy with fluorescein angiography to provide unprecedented clinical measurements of microvascularity in the retina.
2016
With the introduction of OCT angiography, the en face OCT perspective pioneered initially at NYEE, it becomes widely adopted as a tool for monitoring vascular and structural changes in patients with glaucoma, diabetic retinopathy, and macular degeneration at resolution for clinical applications previously available only with adaptive optics.
Drs. Rosen and Chui, under the auspices of NYEE’s David E. Marrus Adaptive Optics Laboratory, translate their work in adaptive optics imaging to OCT angiography, introducing a full spectrum of quantitative tools for precision assessment and follow-up of clinical microvascular disease.
2017
Mount Sinai/New York Eye and Ear (NYEE) Eye and Vision Research Institute is established. As the first of its kind in the New York City metropolitan region, the Institute brings together eye and vision researchers from NYEE, The Mount Sinai Hospital and Icahn School of Medicine at Mount Sinai.
2017
NYEE research studies expand to include more than 100 clinical, translational, epidemiological, and bench investigations under the direction of faculty and trainees.

2017
The Ear Institute at New York Eye and Ear Infirmary of Mount Sinai, led by Drs. George Wanna and Maura Cosetti, are the first to use the newly approved/released SlimJ electrode in the Northeast.
The Ear Institute introduces the transcanal endoscope ear surgery and the endoscopic surgery of the lateral skull base using the exoscope, a cutting-edge extracorporeal video microscope.
2018
Building upon earlier work in adaptive optics, Drs. Rosen and Chui, under the auspices of NYEE’s David E. Marrus Adaptive Optics Laboratory and in collaboration with Dr. Joseph Carroll from the Medical College of Wisconsin, develop the first normative data for OCT angiography, facilitating recognition of quantitative abnormalities retinal blood flow.
2018
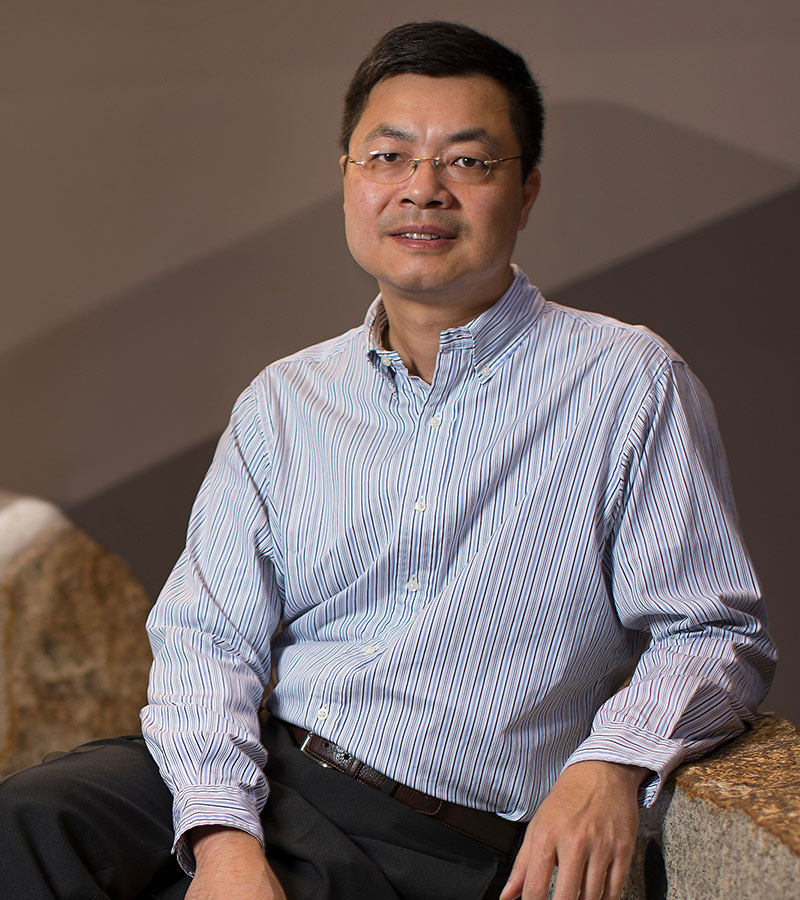
Mount Sinai/NYEE Eye and Vision Research Institute’s Dr. Bo Chen demonstrates how the gene transfer of ß-catenin and three transcription factors in a living mouse can successfully reprogram retinal glial cells into rod photoreceptors, enabling congenitally blind mice to see light for the first time.

2019
NYEE and The Mount Sinai Hospital merge their ophthalmology residency programs to form the largest ophthalmology residency program in the nation.

2020
Tsontcho A. Ianchulev, MD, at NYEE, in collaboration with the Dutch developer of Preceyes Surgery System, introduces the first robotic interventional system for ocular surgery in the U.S., ushering in a new era of unlimited potential in precision surgery. The first micro intervention robotic eye surgical system was installed at NYEE in August 2020.

2020
R. Theodore Smith, MD, PhD and his team developed a family of artificial intelligence (AI)-driven models that, for the first time, can identify not only patients at risk for age-related macular degeneration (AMD), but also those who are likely to progress to late-stage AMD within one to two years and should be seeking ophthalmic care.
2021
Research team led by Timothy Blenkinsop, PhD at the Mount Sinai/New York Eye and Ear (NYEE) Eye and Vision Research Institute found that retinal cells derived from the eyes of human cadavers are able to survive and partially regain their function when transplanted into the maculae of non-human primates. By taking advantage of eye donations, the cadaver-derived ocular cells offer a distinct opportunity for donor compatibility with a virtually unlimited supply. Another special attribute these cells have is they have lived a lifetime as RPE and therefore may be more mature and stable than other stem cell sources.
2021
For the first time Drs. Rosen and Chui, under the auspices of NYEE’s David E. Marrus Adaptive Optics Laboratory, have demonstrated how OCT (optical coherence tomography) angiography can be used to evaluate the immediate status of sickle cell disease using dynamic retinal imaging that depicts microscopic changes in blood flow in the smallest blood vessels. This approach allows for noninvasive monitoring of the retinal microcirculation over time and assessment of a sickle cell patient’s condition before or after initiation of therapy.
2021
Bo Chen, PhD describes how the reactivation of a key enzyme known as CaMKII and its downstream signaling in retinal ganglion cells through gene therapy provides robust protection of retinal ganglion cells and preserves vision in multiple diseases and injury mouse models.
2021
Retinal imaging took another bold leap at NYEE with the development of non-confocal adaptive optics processing that allows for visualization of the eye’s microvasculature down to capillaries and the aneurysms that develop in diabetes and hypertension. The new enhancement to adaptive optics scanning light ophthalmoscopy (AOSLO) by Toco Chui, PhD, allows us to see microscopic structures and cellular-level movement with a resolution and clarity never before possible.
2022
Using retinal imaging of patients, a multidisciplinary team of researchers, R. Theodore Smith, MD, PhD, Richard Rosen, MD, and Jagat Narula, MD, PhD discovered a new connection between subretinal drusenoid deposit (SDD) form of age related macular degeneration (AMD) and high risk vascular diseases such as stroke and cardiovascular disease.
2022
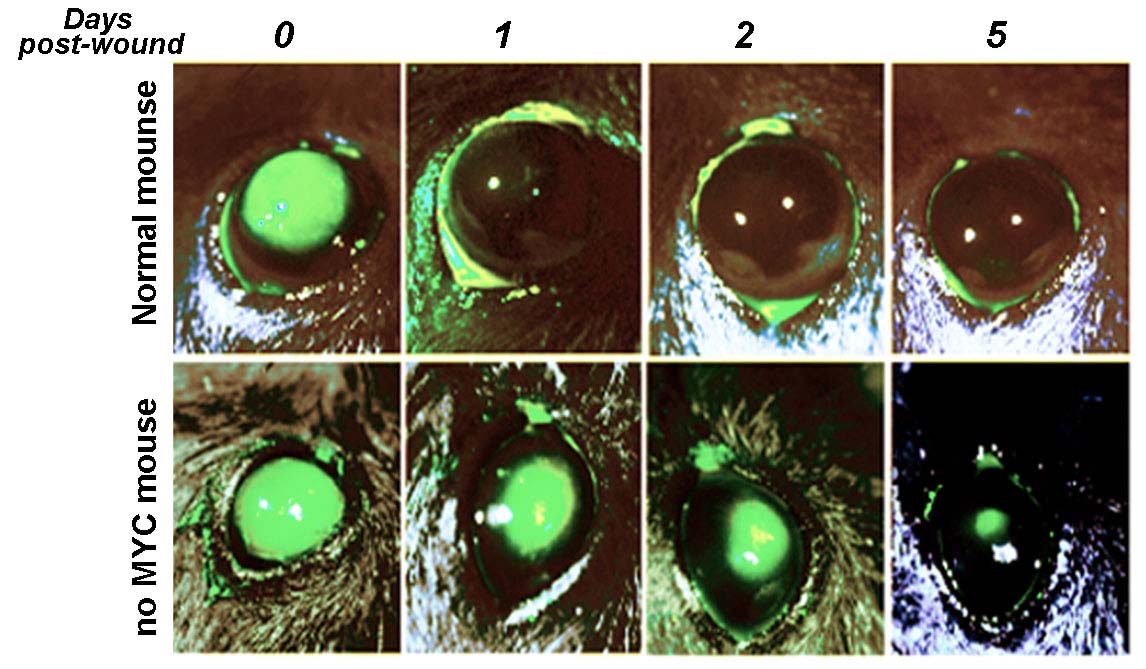
For the first time, the Icahn School of Medicine at Mount Sinai researcher Mario Wolosin, PhD, FARVO, and a team of scientists from Wilmer Eye Institute, and Johns Hopkins University School of Medicine has found that c-Myc is a critical mediator of the proliferative response that limbal stem cells mount when rapidly repopulating the ocular surface if a physical, chemical, or other type of injury occurs, opening the door to improving the generation of transplantable limbal stem cell sheets to treat limbal stem cell deficiency and restoring the damaged corneal surface.
2022
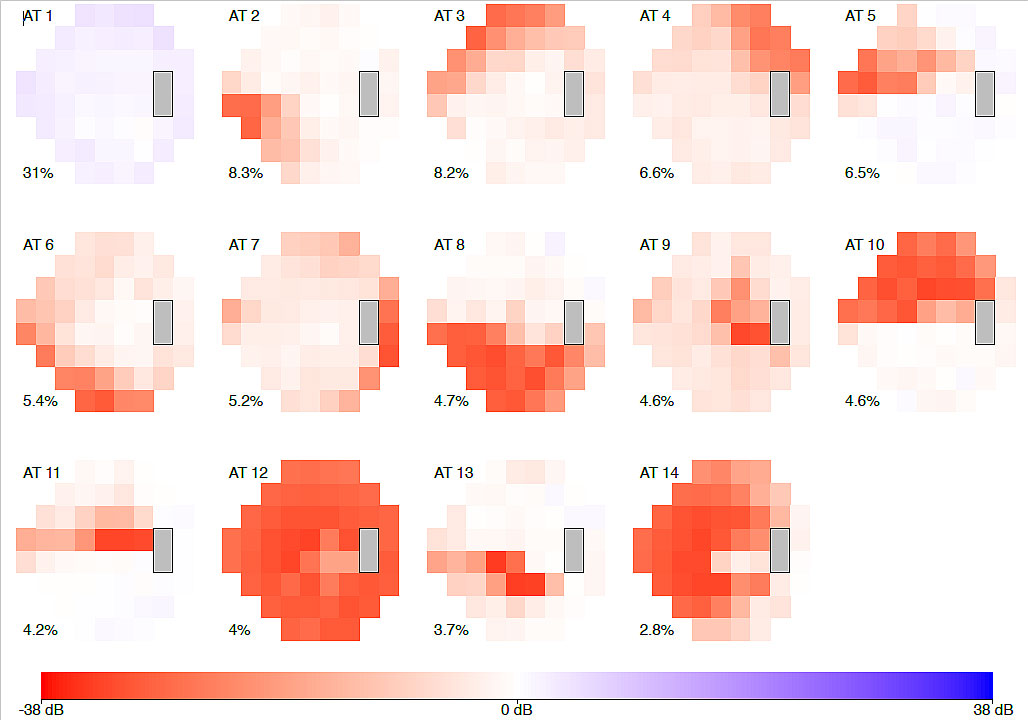
Using archetype analysis, a form of artificial intelligence (AI), to new-onset visual field loss associated with primary open-angle glaucoma (POAG), Louis R. Pasquale, MD, at NYEE in conjunction with collaborators at Brigham and Women’s Hospital and Massachusetts Eye and Ear, uncovered 14 visual field loss patterns ranging from mild peripheral loss to advanced damage across the entire field of vision. The results, showed that Blacks were at a significantly higher risk of POAG with early advanced functional damage compared to non-Hispanic whites.
2023
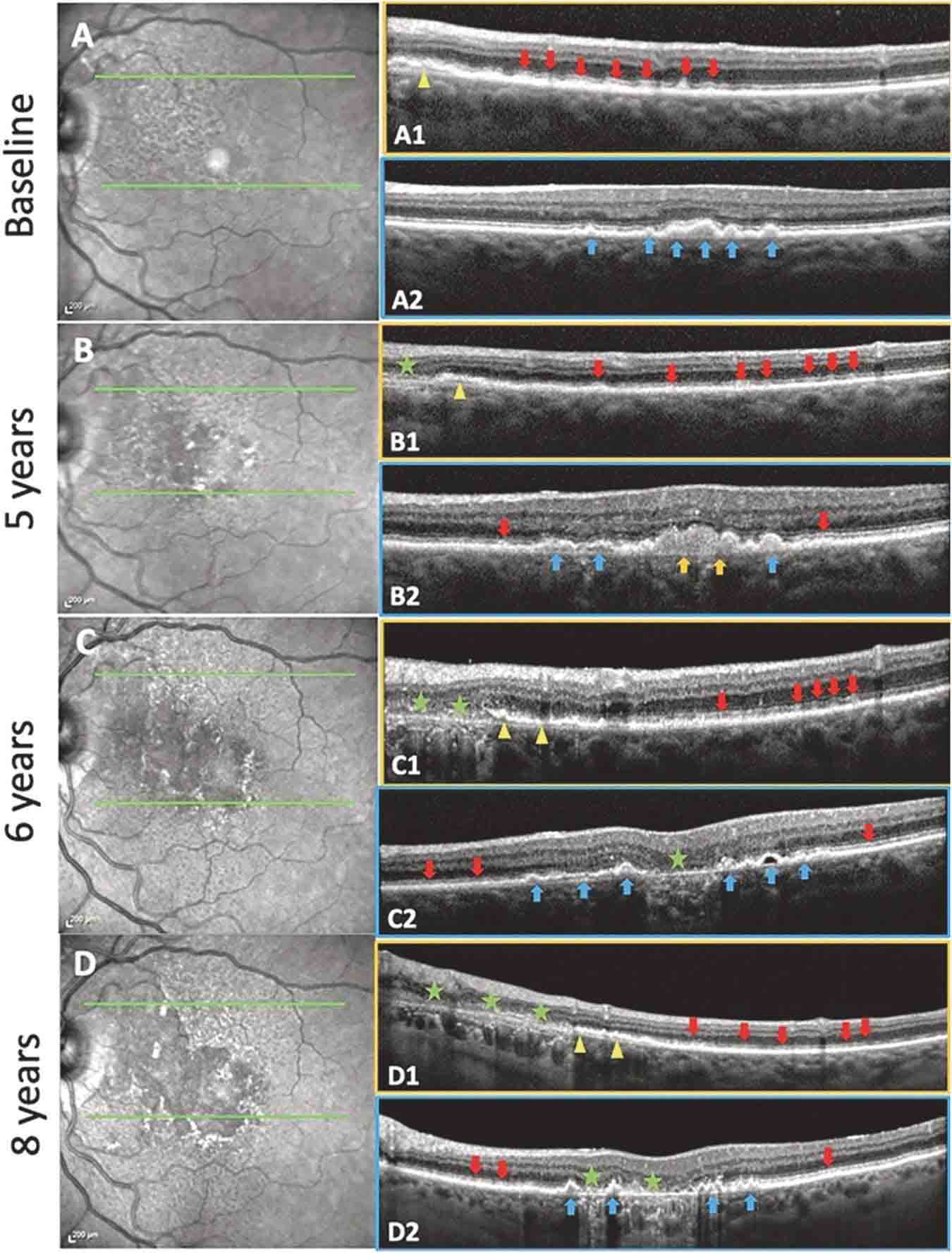
Using autofluorescence measurements and OCT scans, NYEE investigators were the first to demonstrate that two different types of deposits (drusen and subretinal drusenoid deposit, SDDs) in the retina are two different diseases that can contribute to early age-related macular degeneration (AMD), which can progress to advanced AMD and blindness. The findings of R. Theodore Smith, MD, PhD and a team of Mount Sinai researchers mean that these two diseases could be diagnosed, studied, and treated separately with appropriate early intervention to prevent vision loss and other complications.

2023
NYEE launched the Center for Ophthalmic Artificial Intelligence and Human Health, the first of its kind in New York and one of the first in the country. The Center is aimed at making breakthroughs in AI-driven diagnostic and clinical care of eye disease that can benefit patients personally as well as on a much broader population scale.
2023
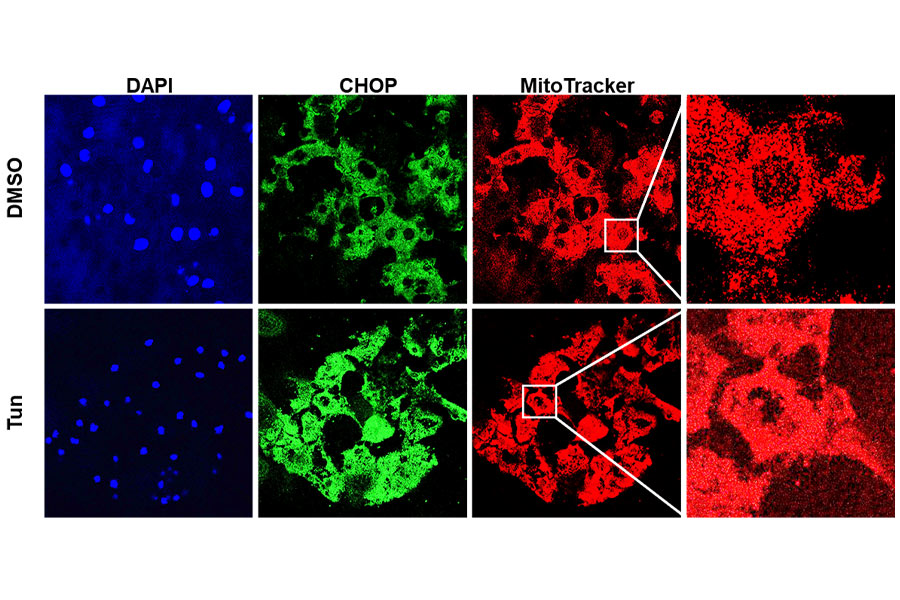
Varun Kumar, Ph.D., and his team of researchers at NYEE described for the first time the three protein-signaling pathways that are activated when endoplasmic reticulum stress disrupts mitochondrial bioenergetics, resulting in corneal endothelial cell apoptosis. The work has implications for not just ocular but neurodegenerative, cardiovascular, and metabolic diseases where such "crosstalk" has also been reported.
2023
Bo Chen, PhD and his research team developed two powerful new tools for in vivo delivery of neuronal factors to reprogram glial cells in the retina or the brain after other studies showed the ineffectiveness of a gene transfer approach once deemed highly promising by the field. The two new AAV-driven gene transfer systems are able to deliver a range of programming factors, and combinations of factors, to glial cells in the retina and brain, with significantly reduced leakage—making gene transfer therapy work more effective.
2023
NYEE researcher team, led by Richard Rosen, MD, showed that measuring changes to flavoprotein fluorescence (FPF) in the optic nerve of people at various stages of glaucoma could set the stage for a critical new prognostic tool to potentially head off glaucoma before it can cause cell loss and structural damage to the optic nerve—damage that remains irreversible. The study is the first to show that FPF may be an important objective measure for predicting glaucoma progression at an early stage, compared to measuring structural damage at the optic nerve head after it’s occurred.

2024
NYEE was one of only 10 Centers in the US (the first in New York) to introduce the newly FDA approved micro-interventional phaco-free cataract technology (miCOR). The first clinical cases took place in January 2024 with Kira Manusis, MD using the subsonic cool-tip lenspen, miCOR on five cataract patients. Developed by Sean Ianchulev MD, MPH, Director of the Ophthalmic Innovation and Technology at NYEE, the micro-interventional subsonic lensectomy allows surgeons to perform cataract surgery using a subsonic lens-pen with no cavitation, low energy, low flow and without the need for a phacoemulsification console.